Gadolinium toxicity
What is it and is contamination of the COVID-19 shots with gadolinium a possibility?
Quick and dirty answer: Yes, it’s possible but… read on…
Gadolinium (Gd) can occur as a micro-pollutant from hospital waste, derived from contrast agents used in magnetic resonance imaging (MRI) in humans. In addition to contamination of water supplies and food from waste release, direct intravenous injection of such contrast agents can lead to bioaccumulation and subsequent gadolinium toxicity, leading to potentially severe life-threatening pathologies involving systemic fibrosis.
The consequences of gadolinium-based contrast agent accumulation on human health have not been evaluated. Gadolinium is a micro-pollutant, largely from hospital waste. B. Wagner, M.D.
Although gadolinium can be ingested via drinking water, exposure is far higher in the context of intravenous injection where an 8-fold higher exposure is reported to occur.12 Evaluations of gadolinium toxicity, such as accumulations in bone from direct intravenous injection, have been done but more studies are certainly required.3456789
What is gadolinium?
gadolinium (Gd), chemical element, a rare-earth metal of the lanthanide series of the periodic table.
Gadolinium is a moderately ductile, moderately hard, silvery white metal that is fairly stable in air, although with time it tarnishes in air, forming a thin film of Gd2O3 on the surface.10
What is a gadolinium chelate?
The word chelation is derived from Greek χηλή, chēlē, meaning "claw"11 and so a gadolinium chelate is a macromolecule that holds the gadolinium ion. Think back to when we talked about hemoglobin: the porphyrin ring is an iron chelate. Below is a diagram of the Gd (macrocyclic) chelate otherwise known as Dotarem.

What is gadolinium or gadolinium chelate used for in humans?
Gadolinium chelates are widely used as contrast media for magnetic resonance imaging. The approved gadolinium-based contrast agents (GBCAs) have historically been considered safe and well tolerated when used at recommended dosing levels.12
Clinically available gadolinium chelate-based contrast agents (GBCAs) are divided into two groups by chelate types: linear GBCAs and macrocyclic GBCAs.13
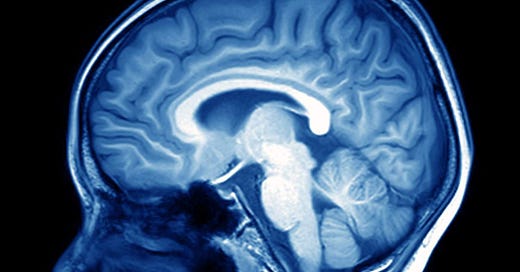
What are MRIs?
MRIs are cross-sectional diagnostic imaging modalities that avoid the issues with previous imaging modalities like ionizing radiation. In addition to enhanced 3D images, improved contrast agents (CAs) also allow for better and safer imaging for diagnostic purposes. You can read about CAs here.14 GBCAs are used as CAs because of their excellent paramagnetic properties.15 Here's a good question and answer document on MRIs and GBCAs.

So if you’ve ever had a contrast MRI, then likely you’ve been intravenously-injected with a gadolinium chelate like the linear chelate Gadopentetate dimeglumine, Gd-DTPA (Magnevist) or the macrocyclic chelate Gadobutrol (Gadovist). The benefit of the macrocyclic chelate version is the comprehensive cloaking of gadolinium itself, the minimization of the chances of its release and subsequent toxicity potential,16 and the enhanced molecular stability.1718 Below are comparative diagrams of examples of linear (Magnevist) and macrocyclic (Dotarem) chelates. See how snuggly the Gd+3 is on the right?
Problems potentially arise when gadolinium detaches from its chelator molecule and becomes free. This is when the issue of gadolinium toxicity can arise. Gadolinium toxicity is commonly accompanied by nephrogenic systemic fibrosis (NSF): a kidney-associated induction of systemic fibrosis.19 NSF is especially problematic for people with impaired kidney function, but not exclusively so.20 NSF is characterized primarily by skin fibrosis (skin becomes thicker and harder), but can also involve subcutaneous tissue fibrosis and even skeletal and smooth muscle fibrosis. The immunopathology is something of a continuing mystery but likely involves 'dysregulation' of fibrocytes - 'hematopoietic-derived cells that directly contribute to tissue fibrosis by producing collagen following injury, during disease, and with aging'.2122 Fibrocytes are the inactive form of fibroblasts. That clears it up, eh?
This proliferation of fibrotic tissue may become systemic, extending to other areas including the smooth, delicate membrane that surrounds the lungs (pleura), the sac surrounding the heart (pericardium), the thin sheet of muscle that aids respiration by moving up and down when breathing (diaphragm), and the outermost layer (dura mater) of the three membranes covering the brain and spinal cord.23
Gadolinium deposition can also occur in the brain, bones, testis and other tissues.2425
Gadolinium toxicity can be associated with a wide-range of clinical symptoms. In a survey completed by the Gadolinium Toxicity.com group to assess the frequencies of the chronic effects of retained gadolinium (See Survey of the Chronic Effects of Retained Gadolinium from Contrast MRIs), the surveyors found the following associated adverse events reported frequently:
Pain – aching; burning, tingling, and/or prickling pain (paresthesia); deep bone pain.
Dermal changes – like tight skin, lesions, hyperpigmentation.
Muscle issues – twitching – small, local, rapid contractions and weakness
Ocular problems – worsening vision, dry eyes, bloodshot eyes
Cognitive symptoms
Ear, nose and throat – tinnitus, swallowing, and voice problems
Low body temperature
Hair loss (alopecia)
Itchy skin (pruritus)
Balance problems
Swelling of extremities (edema)
Up to this point, I haven’t mentioned anything about the adverse events that I have been extensively studying for over 2 years. But in addition to the sheer number of AE reports that have been filed in the context of the COVID-19 shots, I have been paying close attention to the range and types of AEs, and the systemic nature of the AE occurrences. I have also taken up a keen interest in the fibrotic associated AEs and amyloid formation. And after reading the following, I had to ask myself, are there shared immunopathologies between iatrogenic fibroses seen between the NSF-related Gd toxicity and the AEs reported in association with the COVID-19 shots? Read on…
There is one symptom experienced by many that transcends several of the symptoms listed above. It is a sense of an electrified, vibrating, twitching feeling typically just under the skin that is sometimes localized and at other times a more overall feeling. Sometimes it feels like something is crawling around under the skin. This is a particularly alarming feeling when first experienced as it is unlike anything that the person has ever experienced and it is very difficult to explain to doctors.
This last paragraph is quoted verbatim from the gadoliniumtoxicity.com website is reminiscent of many anecdotal accounts of AE occurrences following the COVID-19 injections. The reason this struck me is due to the fact that pre-COVID, I hadn't heard of a feeling of being electrified as a commonly-reported side effect of a 'vaccine'. These are the only 2 contexts I have read about this. Read on…
The physiological basis behind why people can experience muscle involvement (including twitching) in the context of Gd toxicity, is due to the fact that gadolinium competes biologically with calcium - it blocks voltage-gated calcium channels. Just some of the physiological effects of this blocking includes inhibition of smooth, skeletal, and cardiac muscle contraction, inhibition of transmission of nerve impulses and blood coagulation. Gadolinium can also inhibit mitochondrial function and induce oxidative stress.2627 It can get into bones by competing with calcium based on similarities in ionic radii (for example), where it can stay for many, many years.28 [The ionic radius of Gd+3 (108 pm) is very close to that of Ca+2 (114 pm).]
There are currently 7 GBCAs approved for clinical use. They are injected at ‘low’ doses between 0.1–0.3 mmol/kg body weight.29 Except for one, of which about half goes straight to the liver, most of the agents get disseminated in the extracellular interstitial space. If you ask me, any amount could be considered high enough to induce gadolinium toxicity since a) it is a toxic heavy metal that doesn’t belong in the body and b) we don’t know exactly why, where or how accumulation occurs, or the manner in which it does so. Remember the words of Paracelsus: “Solely the dose determines that a thing is not a poison.” Perhaps the dose requirement for poisoning is really small in some people - say, people with poor kidney function. :)
Naturally, the likelihood of accumulation and toxicity increases with repeated and higher doses, the specific GBCA used, and the pre-condition of the organs of the individual. When kidney function is normal, elimination of GBCAs is thought to occur in less than 2 hours after intravenous injection, and more than 95% is thought to be eliminated within 24 hours. It is important to remind everyone, however, that it has also been shown that even when the kidneys are functioning properly, toxicity can occur from accumulation in the brain. [Kanda et al., 2015]
I think it’s time for some calculating. Just, because I like thinking about things in terms of particles. Let’s look at gadobutrol as a specific example of a clinically-used GBCA. Gadobutrol has a molar mass of 604.72 g/mol. That means that the mass of 1 mole of gadobutrol is 604.72 grams. So since there are 6.02x10^23 particles in 1 mole of any elementary entity, then there are 6.02x10^23 particles in 604.72 grams of gadobutrol. The minimum recommended dose of gadobutrol is 0.11 mmol/kg or 0.00011 mol/kg. So if we inject this amount into a 60 kg person, then they will get a dose of 0.00011 mol/kg * 60 kg * 6.02x10^23 = 3.97x10^21 particles of gadobutrol. It has been shown that 0.7% of people sustain an adverse event (0.03% are considered serious) at this minimum recommended dose, with rates as high as 2.5% in ‘at-risk’ individuals.30
One patient experienced a fatal anaphylactoid shock, assessed to be related to injection of gadobutrol.31
The accumulated safety record [for GBCAs] is excellent, with serious adverse reactions occurring in roughly 0.03% of all administrations. These adverse reactions are more common in patients with history of asthma, allergies, and renal insufficiency and in patients injected at faster rates.3233343536
So, if we injected 10,000 people, 3 would suffer a severe AE. Therefore, at these low doses, those aren’t bad odds at all, and by the above calculations a ‘baseline’ of 3.97x10^21 particles of gadobutrol is enough to induce severe AEs in 3/10,000 people. So the question again becomes, why do things go awry in these 3 people? Is it something specific about their physiologies beyond kidney problems? Are they simply examples of acute onset reactions where the majority of people don’t see the effects of Gd toxicity until a later time point?
As mentioned above, 5% of the original number of GBCA particles are not filtered by the kidneys within the first 24 hours, meaning that ~1.9x10^20 particles remain thereafter for an unknown amount of time. The longer these particles are in the body, the higher the chances of dissociation from their Gd ion (especially in the case of linear GBCAs) to subsequently undergo deposition in various places in the body, like the bones and the brain. So the more refined question becomes, do the AEs arise in the 0.7% due to distribution and deposition of the free Gd resulting from the 5% that does not get filtered in the first 24 hours? It’s likely that some threshold of Gd needs to be attained in order for specific AEs to occur, so toxicity really depends both on time and accumulation achieved by multiple dosing.
Let’s return to NSF for a moment. Shawn Cowper of Yale has documented many cases of NSF37 associated with gadodiamide, a linear GBCA. Even though NSF pathogenesis is not entirely clear, according to Cowper, it likely involves the migration of CD34 (an important adhesion molecule) and procollagen-1 (a marker of fibroblastic and fibrohistiocytic skin tumors)38 positive circulating fibrocytes from the blood to affected tissues. Fibroblast proliferation in tissues examined from healthy subjects was found to be stimulated by all GBCAs.39 This is a remarkable statement and indicates wound healing 'processes' and all related goodies like collagen and the extracellular matrix stuff are activated and stay activated due to the presence of Gd. Remember that this immune system thing is one nosy nelly and is an integral part of all physiological responses so we have to factor in all of the chemotactic factors, cytokines and inflammatory mediators.
Several reports have shown increased expression of transforming growth factor β1 (TGF-β1) and CD68-factor XIIIa within the affected skin and skeletal muscle which are also essential markers associated with wound healing and fibrosis.4041
Remember how we talked about TGF-β as the master regulator of organ fibrosis?
An extension of NSF (just exploratory)
I have written about the problems associated with fibrosis and collagen over-production before in the context of VAERS reports for COVID-19 shot-related AEs. To be clear, I did do a query for gadolinium in VAERS (which I will summarize in the next paragraph) but there is nothing to suggest that there is actually gadolinium in the shots causing the AEs. If you were wondering. I was. I also spoke to a panel of experts who did heavy metal toxicology screens of the COVID-19 injectable products (4 vials of Moderna) and no gadolinium was detected by their analysis. Granted, it was a small sample size and not specifically seeking this metal, but still.
Having said that, however, since I have been learning about fibrosis now from these two points of view, I must wonder about similar pathways/pathologies leading to fibrosis-related AE occurrences (and others like tinnitus and ‘electrification’) that are seen in both the cases of gadolinium deposition, and in association with exposure to the shots. In the case of gadolinium toxicity, we know, at least, that wound healing goes into overdrive in people with kidney problems who can’t properly filter out free gadolinium, but what’s in the COVID shots that’s egging on fibrosis, and in fact, inducing a wildly comprehensive range of AEs including all of the above?
To satisfy my curiosity concerning the potential for gadolinium deposition from the shots (one way or the other), I did a query in VAERS using the keyword ‘gadolinium’. My query returned 570 VAERS IDs with this keyword looking in the following variables: CUR_ILL (current illnesses), ALLERGIES, SYMPTOM_TEXT, HISTORY or LAB_DATA. None of these reports were actually reported as AEs. Half of the returned IDs involved gadolinium used for cardiac MRIs in individuals with suspected myocarditis. Gadolinium deposition disease/toxicity was previously reported in 27 individuals. I have to ask, why on Earth would anyone get injected with an experimental product if they had known gadolinium toxicity issues? I wish people were given true informed consent.
125 of these people had reported allergies to gadolinium. These individuals interested me. What kind of reactions did they have, for example? Any anaphylactic reactions? Was fibrosis an issue? It was reported previously that individuals suffering anaphylaxis in the context on the Moderna shots had gadolinium allergies. Maybe these same people just had higher allergic proclivity to a bunch of things, including gadolinium, but maybe the anaphylaxis was in response to PEG exposure?
Indeed, 7 individuals who had gadolinium allergies had anaphylactic shock written down as an AE, but perhaps even more interesting is that 50% of the 125 individuals with the known gadolinium allergy reported their AEs within the first 24 hours. Sounds like acute reactions to me. These AEs ranged from Bronchospasm to Chills.
In spite of these interesting tidbits from VAERS, I can’t say there’s anything really ‘incriminating’ about what I found. So, the quick and dirty answer to the title question “Is contamination of the COVID-19 shots with gadolinium a possibility?” is: Yes it is, but based on the small evidence pool I have access to, for now, I don’t think gadolinium contamination is an issue with the COVID-19 shots. It was a nice idea, and perhaps still is conceptually from a heavy metal point of view, because there is something, perhaps many things, in the shots wreaking havoc - I mean, apart from spike. Maybe. I know the spike is inducing self-damage and thrombotic issues, but what of the brain, specifically? Is there something else inducing neurological issues apart from spike? Sorry for being vague. Sometimes I have to be because my bandwidth is low. And speaking of heavy metal:
Some of you might be wondering why I decided to write a Substack about gadolinium. And Metallica. I was familiar with it only from the reference to gadolinium enhancement as LAB_DATA in some VAERS reports from a previous manuscript that I penned. I started reading about gadolinium toxicity and was struck by the systemic nature of the damages that this rare earth metal was able to impose on the human body. It’s wild how much damage things can do if they’re not meant to be there. It’s also wild how amazing the body is in and of itself and if left alone, it can heal.
Ultimately, like all things in nature, the immune system and treatment, all things in moderation. Right? Too much, or perhaps too little (of such things like surfing) of anything is bad, in my opinion. Take the agenda of COVID injectors as an example. Injecting an entire species with the same thing regardless of age, health status, race, etc… is a profoundly stupid idea and if your intention is to mindlessly ‘vaccinate’ everyone without knowing squat about immunology, epidemiology, vaccinology or virology, then trust me, you’ll learn pretty fast why that’s idiotic.
I agree with Paracelsus on his ideas about toxicity (that the dose makes the poison) and about a great many other things. For example, he believed that things that look like things, heal things. Bulbs, because they look like testicles, could have healing properties for infertility? Sounds like awesome thinking to me. Seriously. Not kidding. Think about the mathematics of things - the ratios.
Time can heal all wounds. Except if you’re talking about something that increases wound healing to the point where it becomes pathological. Like gadolinium. Alrighty then. Before I start making fun of myself, I will post this article with a promise to follow-up if I find anything interesting.
Kulaksız S and Bau M 2011 Anthropogenic gadolinium as a microcontaminant in tap water used as drinking water in urban areas and megacities Appl. Geochem. 26 1877–85.
Lord, M. L., McNeill, F. E., Gräfe, J. L., Noseworthy, M. D., & Chettle, D. R. (2018). Self-identified gadolinium toxicity: comparison of gadolinium in bone and urine to healthy gadolinium-based contrast agent exposed volunteers. Physiological Measurement, 39(11), 115008. doi:10.1088/1361-6579/aaedc6.
Darrah T H, Prutsman-PfeifferJJ, PoredaRJ, Ellen Campbell M, Hauschka PV and HanniganRE 2009 Incorporation of excess gadolinium into human bone from medical contrast agents Metallomics 1 479–88.
Grobner T 2006 Gadolinium: a specific trigger for the development of nephrogenic fibrosing dermopathy and nephrogenic systemic fibrosis? Nephrol. Dial. Transplant. 21 1104–8.
Kanda T, IshiiK, Kawaguchi H, KitajimaK and Takenaka D 2014 High signal intensity in the dentate nucleus and globus pallidus on unenhanced T1-weighted MR images: relationship with increasing cumulative dose of a gadolinium-based contrast material Radiology 270 834–41.
Kanda T, Fukusato T, Matsuda M, ToyodaK, Oba H, Haruyama T, KitajimaK and Furui S 2015 Gadolinium-based contrast agent accumulates in the brain even in subjects without severe renal dysfunction: evaluation of autopsy brain specimens with inductively coupled plasma mass Radiology 276 228–32.
Keldani Z, Lord M L, McNeill F E, Chettle D R and Gräfe J L 2017 Coherent normalization for in vivo measurements of gadolinium in bone Physiol. Meas. 38 1848–58.
Huckle J E, Altun E, Jay M and SemelkaRC 2015 Gadolinium deposition in humans when did we learn that gadolinium was deposited in vivo ? Invest. Radiol. 51 236–40.
High WA, Ayers RA and Cowper SE. 2018. Gadolinium is quantifiable within the tissue of patients with nephrogenic systemic fibrosis J. Am. Acad. Dermatol. 56 710–2.
https://www.britannica.com/search?query=gadolinium+
https://en.wikipedia.org/wiki/Chelation
Rogosnitzky M, Branch S. Gadolinium-based contrast agent toxicity: a review of known and proposed mechanisms. Biometals. 2016 Jun;29(3):365-76. doi: 10.1007/s10534-016-9931-7. Epub 2016 Apr 6. PMID: 27053146; PMCID: PMC4879157.
Nakajima, T., & Lamid-Ochir, O. (2020). Current Clinical Issues: Deposition of Gadolinium Chelates. Rare Earth Elements and Their Minerals. doi: 10.5772/intechopen.91260.
Runge VM. Chapter 14. Contrast media BT-clinical MRI. Clinical MRI. 2002:454-472.
J. Ramalho, R.C. Semelka, M. Ramalho, R.H. Nunes, M. AlObaidy, M. Castillo. Gadolinium-Based Contrast Agent Accumulation and Toxicity: An Update. American Journal of Neuroradiology Jul 2016, 37 (7) 1192-1198; DOI: 10.3174/ajnr.A4615
Frenzel T, Lengsfeld P, Schirmer H, Hütter J, Weinmann HJ. Stability of gadolinium-based magnetic resonance imaging contrast agents in human serum at 37 degrees C. Invest Radiol. 2008 Dec;43(12):817-28. doi: 10.1097/RLI.0b013e3181852171. PMID: 19002053.
Runge, Val M. MD. Macrocyclic Versus Linear Gadolinium Chelates. Investigative Radiology 50(12):p 811, December 2015. | DOI: 10.1097/RLI.0000000000000229
https://appliedradiology.com/articles/delivering-stability-with-macrocyclic-gadolinium-based-contrast-agents
Broome DR. Nephrogenic systemic fibrosis associated with gadolinium based contrast agents: A summary of the medical literature reporting. European Journal of Radiology. 2008;66:230-234. DOI: 10.1016/j.ejrad.2008.02.011.
Kanda T, Fukusato T, Matsuda M, Toyoda K, Oba H, Kotoku J, et al. Gadolinium-based contrast agent accumulates in the brain even in subjects without severe renal dysfunction: Evaluation of autopsy brain specimens with inductively coupled plasma mass spectroscopy. Radiology. 2015;276:228-232. DOI: 10.1148/radiol.2015142690.
https://my.clevelandclinic.org/health/diseases/17783-nephrogenic-systemic-fibrosis-nsf
Reinhardt James W., Breuer Christopher K. Fibrocytes: A Critical Review and Practical Guide. Frontiers in Immunology. VOLUME=12. YEAR=2021. doi: 10.3389/fimmu.2021.784401.
https://rarediseases.org/rare-diseases/nephrogenic-systemic-fibrosis/
https://gadoliniumtoxicity.com/help/symptoms/
Kanda T, Fukusato T, Matsuda M, Toyoda K, Oba H, Kotoku J, et al. Gadolinium-based contrast agent accumulates in the brain even in subjects without severe renal dysfunction: Evaluation of autopsy brain specimens with inductively coupled plasma mass spectroscopy. Radiology. 2015;276:228-232. DOI: 10.1148/radiol.2015142690.
Feng X, Xia Q, Yuan L, et al. Impaired mitochondrial function and oxidative stress in rat cortical neurons: implications for gadolinium-induced neurotoxicity. Neurotoxicology2010;31:391–98doi:10.1016/j.neuro.2010.04.003pmid:20398695.
Xia Q, Feng X, Huang H, et al. Gadolinium-induced oxidative stress triggers endoplasmic reticulum stress in rat cortical neurons.J Neurochem2011;117:38–47doi:10.1111/j.1471-4159.2010.07162.xpmid:21198628.
Darrah TH, Prutsman-Pfeiffer JJ, Poreda RJ, et al. Incorporation of excess gadolinium into human bone from medical contrast agents.Metallomics2009;1:479–88doi:10.1039/b905145gpmid:21305156.
https://mriquestions.com/so-many-gd-agents.html
Levine D, McDonald RJ, Kressel HY (2018) Gadolinium retention after contrast-enhanced MRI. JAMA 320: 1853-1854. doi: 10.1001/jama.2018.13362.
Prince MR, Lee HG, Lee CH, Youn SW, Lee IH, Yoon W, Yang B, Wang H, Wang J, Shih TT, Huang GS, Lirng JF, Palkowitsch P; GARDIAN study group. Safety of gadobutrol in over 23,000 patients: the GARDIAN study, a global multicentre, prospective, non-interventional study. Eur Radiol. 2017 Jan;27(1):286-295. doi: 10.1007/s00330-016-4268-8. Epub 2016 Mar 9. PMID: 26960538; PMCID: PMC5127858.
Hao D, Ai T, Goerner F, et al. MRI contrast agents: basic chemistry and safety.J Magn Reson Imaging2012;36:1060–71doi:10.1002/jmri.23725pmid:23090917
Bleicher AG, Kanal E. Assessment of adverse reaction rates to a newly approved MRI contrast agent: review of 23,553 administrations of gadobenate dimeglumine. AJR Am J Roentgenol 2008;191:W307–11 doi:10.2214/AJR.07.3951 pmid:19020220.
Kanal E, Tweedle MF. Residual or retained gadolinium: practical implications for radiologists and our patients. Radiology 2015;275:630–34 doi:10.1148/radiol.2015150805 pmid:25942418.
Ersoy H, Rybicki FJ. Biochemical safety profiles of gadolinium-based extracellular contrast agents and nephrogenic systemic fibrosis. J Magn Reson Imaging 2007;26:1190–97 doi:10.1002/jmri.21135 pmid:17969161.
Lin SP, Brown JJ. MR contrast agents: physical and pharmacologic basics. J Magn Reson Imaging 2007;25:884–99 doi:10.1002/jmri.20955 pmid:17457803.
Deo A, Fogel M, Cowper SE. Nephrogenic systemic fibrosis: A population study examining the relationship of disease development to gadolinium exposure. Clinical Journal of the American Society of Nephrology. 2007;2:264-267. DOI: 10.2215/CJN.03921106.
Krustrup D, Rossen K, Thomsen HK. Procollagen 1 - a marker of fibroblastic and fibrohistiocytic skin tumors. J Cutan Pathol. 2006 Sep;33(9):614-8. doi: 10.1111/j.1600-0560.2006.00484.x. PMID: 16965335.
Piera-Velazquez S., Louneva N., Fertala J. et al. Persistent activation of dermal fibroblasts from patients with gadolinium-associated nephrogenic systemic fibrosis.Ann Rheum Dis2010;69:2017–23doi:10.1136/ard.2009.127761pmid:20570839
Jiménez SA, Artlett CM, Sandorfi N, Derk C, Latinis K, Sawaya H, et al. Dialysis-associated systemic fibrosis (nephrogenic fibrosing dermopathy): Study of inflammatory cells and transforming growth factor β1 expression in affected skin. Arthritis and Rheumatism. 2004;50:2660-2666. DOI: 10.1002/art.20362.
Nakajima, T., & Lamid-Ochir, O. (2020). Current Clinical Issues: Deposition of Gadolinium Chelates. Rare Earth Elements and Their Minerals. doi: 10.5772/intechopen.91260.






I just love you guys. Someone pretty much snobbed me out for being 'a blogger' the other day (as opposed to a recently highly published author of peer-reviewed articles - gee I wonder why not?) and all I wish for them is to know the amazingness and power of Substack information exchange. It is so bloody refreshing and you guys are super high quality peeps.
This is also a remarkably simple, yet powerful statement, which no doubt has 100% agreement among your readership, but which needs to be transmitted to the masses of “educated Westerners” who bought the narrative, trust authority and believe the mantra, “Take it for the common good.”
“Injecting an entire species with the same thing regardless of age, health status, race, etc… is a profoundly stupid idea and if your intention is to mindlessly ‘vaccinate’ everyone without knowing squat about immunology, epidemiology, vaccinology or virology, then trust me, you’ll learn pretty fast why that’s idiotic.”