Interstitial lung disease, MDA5-positive dermatomyositis and ties to SARS-CoV-2 spike protein
Say that 5 times fast...
Someone in the Twitter world tagged me in a post yesterday with an excellent question. He wanted to know if a strange and rare disease that ‘nobody has ever survived’ called MDA5-positive dermatomyositis (anti-MDA5 dermatomyositis), was possibly the result of a ‘wrong immune response’ instigated by the injections. He was asking in the context of a young man who recently died following a diagnosis of anti-MDA5 dermatomyositis. I think another way to ask this question would be to ask if anti-MDA5 dermatomyositis could possibly be the result of an autoimmune reaction instigated by something in the COVID-19 injections. You can click on the screenshot to get to the article about this young man’s death.
Yes, John be good. I do think the injections are instigating autoimmunity, and I think they are doing this by molecular mimicry. It could also be that the spike protein is triggering epigenetic changes to induce these disease states, as I wrote about in my Substack that you can read here.
Before last night, I had no idea what anti-MDA5 dermatomyositis was. Never heard of it. I didn’t know that it was an exceedingly rare autoimmune disease predominantly reported in East Asia, and linked to another rare autoimmune-derived disease called Interstitial Lung Disease (ILD).12 I didn’t know that similarities between its pathology and COVID-19 pathologies had already been described in the literature.3
On MDA5 (melanoma differentiation-associated protein 5)
MDA5 is a protein encoded by the IFIH1 gene in humans that functions as an antiviral effector by pattern recognition receptors (PRRs). In fact, as a member of the intracellular RNA helicase family proteins, it plays a pivotal role in antiviral immune responses. It likes certain viruses. For example, it is documented to ‘prefer’ double stranded RNA (dsRNA) over 2000 nts in length - as in, can detect and bind big cytoplasmic dsRNA - however, it is also activated by ssRNA complexes and positive sense RNA viruses. SARS-CoV-2 is a positive sense ssRNA virus.4
MDA5 is able to detect replicative intermediates of positive sense RNA viruses.5
Antibodies against this protein, aka: anti-MDA5 antibodies, are associated with amyopathic dermatomyositis and rapidly progressive ILD. Symptoms usually include muscle involvement6 and skin rashes (Gottron's papules7, heliotrope rash8).
On ILDs
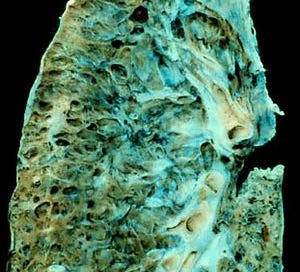
ILDs are a group of disorders that result in lung destruction. The etiology is currently narrowed down to connective tissue disorders, autoimmune diseases or exposures to drugs or exogenous toxins, elements or pathogens.
Interstitial lung diseases (ILDs) are a large group of disorders characterized by thickening of the walls between the alveoli, increased production and buildup of collagen, and pulmonary fibrosis (progressive scarring of lung tissue). The scarring eventually affects the ability to breathe and get enough oxygen into the bloodstream. Symptoms typically include shortness of breath and a dry cough.9

Anti-MDA5 dermatomyositis often leads to ILD and inevitably to death by destruction of lung tissue. Among significant clinical features are spontaneous pneumomediastinum (PNM)[2] and ground-glass opacity (GGO). GGO is observed as a classic clinical COVID-19 marker.1011 It's very serious. And it sounds a lot like COVID-19 to me. As I mentioned, back in 2020, a group published a Letter to the Editor of the European Respiratory Journal entitled: "Similarities between COVID-19 and anti-MDA5 syndrome: what can we learn for better care?" where they wrote:
The hallmark of this disease is the presence of auto-antibodies targeting MDA5, an intracellular sensor of viral RNA (including coronavirus) that triggers the innate immune response. The syndrome is characterized by systemic signs resembling COVID-19, and ARDS is the main cause of death.
They were right, and they were seeking acknowledgement and use of immunomodulatory treatments such as glucocorticoids and immunomodulatory drugs that work against anti-MDA5 dermatomyositis, in the context of COVID-19 since the two pathologies were so similar.
I guess they didn’t get an audience.
This is serious folks. I think the strong links are too strong to look away from here. Once again, the link to collagen defects and/or connective tissue disorders pops up in this context - all linked to autoimmunity. Does the spike protein have a peptide that molecularly mimics MDA5 in humans? Because, that wouldn’t just be evidence - that would explain much of what we are seeing with regard to adverse events being reported in excess in the context of the COVID-19 shots. In any case, based on the extreme rarity of this ‘disease’, it would be very hard to explain away reports in VAERS in the context of the COVID-19 shots, wouldn’t it?
I am currently on the hunt for any potential shared motifs but in the meantime, upon closer inspection of the VAERS data, there are 42 reports of anti-MDA5 dermatomyositis12 and 738 reports of ILD in VAERS as of Jan 6, 2022.13 It is important for me to point out that 1 of these reports involved a person who had "Gottron's papules" written up in her history, but the report indicates two things: that the papules were present “before her first vaccination in early August 2021” and that the adverse event was related to the shots as reported by the reporting physician. So, which is it? And did the COVID-19 make it worse? Here is someone’s account of her experience with the Moderna shot with regard to her Gottron’s papules.
“This was basically a continuation of symptoms from the 1st dose of Moderna. I was seen two days later for another outbreak of Gottron's papules on my hands and feet.” VAERS_ID: 2245853
There are zero, point, zero, zero reports of anti-MDA5 dermatomyositis prior to 2021, and 2 reports of ILD in the past 5 years in the VAERS domestic data set (and 15 since 1990, prior to 2021)14, as compared with 154 reports of ILD in 2021 alone. I am comparing the numbers to 2021 alone because the numbers are presumably ‘all in’ for 2021. Considering there are 77 times more reports of ILD in 2021 for the COVID-19 injectables alone (administered in the U.S.) than for the past 5 years for all vaccines combined, I think this warrants investigation. And combine that again with the fact that anti-MDA5 dermatomyositis has never shown up in VAERS before (as far as I can tell using WONDER - ugh - confirm Liz?), I think this certainly warrants investigation. Yet another safety signal, combined with a therapeutic solution, ignored.
By the way, other clinical markers of anti-MDA5 dermatomyositis include elevated ferritin, C-reactive protein, KL-6, decreased T helper subsets. I did not seek these out in VAERS yet. Also important to nerds, it appears as though anti-MDA5 dermatomyositis is reported by MedDRA code as Dermatomyositis, so it’s vital to seek out the verbatim name in the SYMPTOM_TEXT. I will deep dive into this soon.
I want to publish this now to get y’all thinkin’, and to ask anyone out there who has extra time to confirm or deny a shared MDA5 motif.15 I didn’t find one, but I also didn’t look very hard. I have emailed the corresponding author on the MDPI paper on molecular mimicry that showed a long list of 3D-human mimics found for SARS-CoV-2 spike pentapeptides, just ripe for autoimmunity, entitled: “Potential Autoimmunity Resulting from Molecular Mimicry between SARS-CoV-2 Spike and Human Proteins”. I have found one shared motif that is 4 amino acids long, but I need to look further and get a second opinion.
There was a also paper published in November 2020 that "identified antibodies against immunogenic epitopes with high sequence identity to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in patients of dermatomyositis, suggesting a role of latent viral infection and molecular mimicry in the pathogenesis of DM".16 This got me all riled-up for a second, but upon skimming it, they did not discover a peptide to insinuate molecular mimicry. They also refer to dermatomyositis, and not specifically to anti-MDA5 dermatomyositis.
By the way, before I even got a chance to publish this, the emails started coming in from my Tweet about anti-MDA5 dermatomyositis. Here’s one I literally received just now.
My mom recently died and we haven’t gotten answers to why other than what caused her death, cardiac arrest, failure to thrive and advanced dermatomyositis. We are still waiting for the autopsy results to come back. I understand that this only has 5-6% fatality rate. Unfortunately my mom fired her rheumatologist in Feb because she didn’t like the meds she was given and they 17 side effects they had. But yet was all about getting the death jab and 2 boosters, which personally I feel killed her.
But it’s hard to find any information on this type of autoimmune and the jab.
Yes. It is. We are trying to change that. I wonder if this is anti-MDA5 dermatomyositis?
This is big in my opinion. If autoantibodies are being generated due to the presence of spike against MDA5, then Houston, we have a problem. Like, a big one. The fact that this simply doesn’t appear in VAERS before 2021 is also extremely telling.
So tell everyone.
Kirsty Levasseur, Sofia Tosounidou, Arvind Rajasekaran, Zhia Lim, Catherine McGrath, Priyanka Chandratre, 2. Two cases of anti-MDA5 positive dermatomyositis with rapidly progressive interstitial lung disease, Rheumatology Advances in Practice, Volume 3, Issue Supplement_1, September 2019, rkz026.001, https://doi.org/10.1093/rap/rkz026.001.
Wu W, Guo L, Fu Y, Wang K, Zhang D, Xu W, Chen Z, Ye S. Interstitial Lung Disease in Anti-MDA5 Positive Dermatomyositis. Clin Rev Allergy Immunol. 2021 Apr;60(2):293-304. doi: 10.1007/s12016-020-08822-5. Epub 2021 Jan 6. PMID: 33405101.
Giannini M, Ohana M, Nespola B, Zanframundo G, Geny B, Meyer A. Similarities between COVID-19 and anti-MDA5 syndrome: what can we learn for better care? Eur Respir J. 2020 Sep 24;56(3):2001618. doi: 10.1183/13993003.01618-2020. PMID: 32631836; PMCID: PMC7338399.
Kawaguchi S, Sakuraba H, Haga T, Matsumiya T, Seya K, Endo T, Sawada N, Iino C, Kikuchi H, Hiraga H, Fukuda S, Imaizumi T. Melanoma Differentiation-Associated Gene 5 Positively Modulates TNF-α-Induced CXCL10 Expression in Cultured HuH-7 and HLE Cells. Inflammation. 2019 Dec;42(6):2095-2104. doi: 10.1007/s10753-019-01073-3. PMID: 31440940.
https://en.wikipedia.org/wiki/MDA5
https://understandingmyositis.org/myositis/dermatomyositis/
Ricceri F, Prignano F. Gottron papules: a pathognomonic sign of dermatomyositis. CMAJ. 2013 Feb 5;185(2):148. doi: 10.1503/cmaj.111791. Epub 2012 Jul 23. PMID: 22825999; PMCID: PMC3563888.
https://www.healthline.com/health/skin-disorders/heliotrope-rash#causes
https://rarediseases.info.nih.gov/diseases/13336/interstitial-lung-disease
Maansi Parekh, Achala Donuru, Rashmi Balasubramanya, and Sangita Kapur. Review of the Chest CT Differential Diagnosis of Ground-Glass Opacities in the COVID Era. Radiology. 2020297:3,E289-E302.
Frija-Masson J, et al., Residual ground glass opacities three months after Covid-19 pneumonia correlate to alteration of respiratory function: The post Covid M3 study. Respir Med. 2021 Aug;184:106435. doi: 10.1016/j.rmed.2021.106435. Epub 2021 May 15. PMID: 34020126; PMCID: PMC8123365.
Where keywords: “Anti-melanoma differentiation-associated protein 5 antibody positive” and “Anti-MDA5 dermatomyositis” were sought out in SYMPTOM and SYMPTOM_TEXT columns and where keyword “Gottron’s papules” was sought out in History column to rule it out as a pre-existing condition. My previous search as reported on Twitter was only for “Anti-MDA5 dermatomyositis” that found 12 reports.
By the way, there is another MedDRA code called “Pulmonary interstitial emphysema syndrome” which is probably the same thing as ILD, but I didn’t count these reports.
1 in 2002, 1 in 2005, 1 in 2006, 2 in 2011, 1 in 2013, 1 in 2017, 3 in 2018, 2 in 2019 and 3 in 2020 - as per Interstitial lung disease reports filed to the VAERS domestic data set since its inception.
Mehta P, Machado PM, Gupta L. Understanding and managing anti-MDA 5 dermatomyositis, including potential COVID-19 mimicry. Rheumatol Int. 2021 Jun;41(6):1021-1036. doi: 10.1007/s00296-021-04819-1. Epub 2021 Mar 27. PMID: 33774723; PMCID: PMC8000693.
Gupta L, Chinoy H. Monitoring disease activity and damage in adult and juvenile idiopathic inflammatory myopathy. Curr Opin Rheumatol. 2020 Nov;32(6):553-561. doi: 10.1097/BOR.0000000000000749. PMID: 32890032.





I had my initial ILD exacerbation event two weeks after my first Moderna vaccine jab. I didn’t even put together any sort of correlation in my mind until a month or two ago reading about spike protein causing fibrosis. Two years later I am 90% disabled and on full time O2. Coincidence? ... perhaps. I’ll never know for sure.
Looks like Dr. Sherri Tenpenny will have to add to her list of ways the jabs can kill you. Her list was up to 40 ways last summer and keeps growing. And 88 years ago today little Elvis Aaron Presley was born in a manger in Tupelo. For unto us a child was born, and unto us a son was given. And he would grow up to be the King of Kings of Rock and Roll. And starting tomorrow the W.H.O. is meeting to create a new treaty that will give it power over every country who is a member to declare a pandemic whenever they wish and to force treatments and protocols on everyone in those countries. So Bill will finally have the power to put all the unjabbed in concentration camps and forcefully jab them. And we will all have to have jab passports to do anything. Texas and Alberta may have to secede if this treaty passes.