Spike S1, heparin and the coagulation cascade
Does S1 interfere with coagulation cascade? Does S1 bind to AT-III?
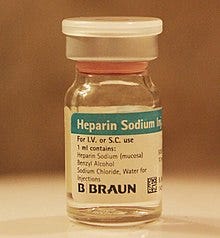
Heparin is a naturally occurring, highly sulfated polysaccharide that plays a critical role in a range of different biological processes. Therapeutically, it is mostly commonly used as an injectable solution as an anticoagulant for a variety of indications, although it has also been employed in other forms such as coatings on various biomedical devices.1

On heparin
A little about heparin(s). I was unaware of most of what I know about heparin now, up until yesterday. To the average person, I would think that heparin is a bit of an unknown. To a medical professional such as an M.D. or a nurse however, heparin is an invaluable exogenous water-soluble solution produced from pigs2 for intravenous administration to humans to resolve such coagulation pathologies as pulmonary embolism or deep vein thrombosis, for example.
Heparins comprise a group of carbohydrates or saccharides that includes unfractionated heparin (UFH), low molecular weight heparin (LMWH) and synthetic heparinoids. Heparin is so-called because it was originally discovered by a medical student in the liver of a dog (from Ancient Greek ἡπατικός (hēpatikós, “of the liver”), from ἧπαρ (hêpar, “liver”3).
Heparin is an endogenous glycosaminoglycan or GAG (a polysaccharide) that comes from mast cells, and works in conjunction with anti-thrombin 3 (AT-III) (a glycoprotein) to induce anti-coagulation effects via inhibition of the coagulation cascade that, when uninhibited, results in the production of fibrin, for example. It does this by binding anti-thrombin 3 (also liver-sourced) which subsequently inhibits the coagulation cascade and thus inhibits production of fibrin. Here’s the coagulation cascade in an instructional video. I am mentioning fibrin because, well, you know.
This is one of the end points of a complex and highly regulated cascade involving many factors. So heparin is a necessary component in a tightly-regulated, highly complex system that regulates clotting. When I learned this, it made me think of the RAAS system. For those of you who haven’t seen my video or read my work on this subject, the RAAS, or the Renin Angiotensin Aldosterone System, is also a tightly-regulated highly complex closed loop system that regulates blood pressure and electrolyte levels. ACE-2 is an essential component in this system. ACE-2 is a membrane-bound (and soluble) protein necessary to induce dilation of the blood vessels following constriction, hence decreasing the blood pressure as part of the loop. ACE-2 is also the primary receptor for the spike RBD. My question remains unanswered: what effect does the presence of the spike protein have on the RAAS? I would assume that any exogenous agent able to act on a constituent of a vital system would enable, or perhaps even ensure, imbalance.
The coagulation cascade reminds me of this. Here’s why.
On heparin binding sites of proteins
The first thing that is important to know is that heparin binding sites exist in many human proteins. You can read about this in this paper: “Heparin-Binding Domains in Vascular Biology” published in 2004.4
Electrostatic interactions play a major role in the binding of heparin to proteins, and basic amino acids such as arginine and lysine are present in the heparin-binding sites of most proteins.
Interesting to me, is that they found that the proteins that bind heparin have positively-charged (at physiological pH) arginines and lysines. They also found high frequency of serines and glycines (nonbasic residues) in heparin-binding peptides. “Both have small side chains, providing minimal steric constrains and good flexibility for peptide interaction with GAG.”
Proteins with heparin binding sites bind heparin. What I want to know is, what effect does this binding have on the coagulation cascade? Is it a normal part of the system? I am still investigating the physiological roles of these proteins.
On heparin binding sites of amyloid-forming proteins
The second thing that is important to know is that of the 20,000 or so proteins of the human proteome, there are more than 25 amyloid-forming proteins that have been identified and associated with serious diseases in humans, and many of these have heparin binding sites including Aβ, α-synuclein, tau, prion and TDP-43 RRM.5 The following table shows 13 human amyloids associated with their respective diseases. For example, the human amyloid beta (Aβ) is associated with Alzheimer’s disease.

A paper published last year entitled: “SARS-CoV-2 spike protein interactions with amyloidogenic proteins: Potential clues to neurodegeneration” suggested that the SARS-CoV-2 S1 RBD binds to a number of aggregation-prone, heparin binding proteins.6 To me, the paper is stunning and alarming. They use docking software to show high affinity binding between the RBD of the S1 portion of the spike protein and Aβ, α-synuclein, tau, prion and TDP-43 RRM.
These interactions suggest that the heparin-binding site on the S1 protein might assist the binding of amyloid proteins to the viral surface and thus could initiate aggregation of these proteins and finally leads to neurodegeneration in brain.
The authors show evidence that S1 binds to amyloid proteins with heparin binding sites, and that’s wild because as they state, this could enhance neurodegeneration. This in and of itself is frightening news and could very well implicate the spike with amyloidosis. But what I want to know is, what exactly happens physiologically when S1 binds heparin and does this binding interfere with downstream effects in the coagulation cascade? Let’s pose this as a research question:
Does the presence of exogenously-introduced endogenously-produced spike protein inhibit the coagulation cascade via S1 by a) binding AT-III or b) binding heparin and thus interfering with downstream anticoagulation effects or c) both?
If it did, we would see bleeding. Among other things.
On spike (S1)
Just to remind everyone, the spike protein of SARS-nCoV-2 comprises two parts: S1 and S2 subunits. That little section in between the S1 and S2 subunits is called a furin cleavage site and is unique to SARS-nCoV-2. It was put there and it makes the virus much more infectious.

S1 protein has been found in individuals in the context of COVID-19 and post-injection with COVID-19 products.7 8 9


So we know that S1 is around. The authors in the aforementioned paper show that the molecular docking score of S1 to heparin is very high (docking energy score: −282.57) as shown in Figure 7. This means that S1 likely binds to heparin with high affinity. An interesting question for me now becomes, since SARS-CoV-2 Spike S1 protein receptor binding domain (SARS-CoV-2 S1 RBD) binds to heparin with even higher affinity than the amyloidogenic heparin binding proteins as shown in Figure 7, what comprises the binding site? Is it arginine (Arg), lysine (Lys) serine (Ser) and glycine (Gly) rich? According to the paper, “the docking results showed that interaction of S1 with heparin is strongly mediated by H-bonds formed by residues Asn354, Arg355, Lys 356, Asn394, Tyr396, and Arg466”. So we have 2 arginines and a lysine out of 6 residues which I suppose might qualify as arginine rich. 1/3 ain’t poor.

On AT-III binding
AT-III is a protein secreted by the liver that binds to heparin to inhibit thrombin and subsequent coagulation cascade events. The result is bleeding. AT-III binds to a specific pentasaccharide (5 sugars) sulfation sequence contained within heparin showed in the following beautiful Pymol images.10

When the pentasaccharide complex binds AT-III, it induces an allosteric conformational change in the protein to purge two prolines from the inside to the outside of the structure, thus manifesting the inhibitory version of the protein which results in inhibition of the coagulation cascade (Figures 8, 9). Allostery is out of this world.

Alright so what do we know? We know that S1 binds with high affinity to heparin. We also know that the mechanism of action of the COVID-19 injectable products is delivery of coding material for the spike protein to be produced en-masse by the host cells. We also know that the lipid nanoparticles (LNPs) biodistribute heavily, and thus production of spike protein happens everywhere in the body. We know that some S1 is found circulating in people post-injection and post-COVID-19. We also know that the spike protein is cleaved at the furin-cleavage site to produce S1 and S2 portions, in the case of the viral form. Does the spike protein encoded by the mRNA contain the furin cleavage site as well?
What will be the effect, in the physiological context, of mountains of spike protein being produced and circulating post injection of COVID-19 injectable products? To me, it is easy to imagine that S1 protein would be cleaved and circulating in both post-COVID and post-injection settings. It is also easy for me to imagine that this S1 would bind endogenous heparin. It also seems highly likely, therefore, that this binding would interfere with heparin’s ability to bind AT-III which means, inhibited coagulation cascade which means: bleeding. The question remains: does S1 bind AT-III directly? Does it even need to since it likely inhibits the coagulation cascade (in any case) due to its bindability with heparin?

I am going to leave this as an open question for now because I want to publish this article, but let me leave you with some VAERS reports reflective of a dysregulated coagulation cascade. This paper here will have some answers as well.11
Heparin-induced thrombocytopenia
One more important point. Heparin-induced thrombocytopenia is the development of thrombocytopenia (a low platelet count), due to the administration of various forms of heparin. So this happens when one has been been previously exposed to heparin and an autoimmune reaction to platelet factor IV. When platelet factor IV combines with heparin on the surface of a platelet it becomes immunogenic. The antibodies against the complex can do two things: it can tag the platelets for destruction by the spleen or it can activate the platelet. What happens then? Platelets do what platelets do! They call more platelets over and have a platelet clot party. So what’s the end result of these two things students? Platelet loss! Which is thrombocytopenia. These clots can cause deep vein thromboses, pulmonary embolisms, myocardial infarctions, cerebrovascular accidents or cerebral venous thrombosis or acute arterial occlusions leading to limb gangrene.
It occurred to me that this might be the difference between people who bleed and people who clot. It would be very interesting to find out who of the people with thrombocytopenia had previously been administered heparin. Furthermore, shouldn’t the shots be counter-indicated in people with bleeding disorders if in fact the spike S1 protein binds to heparin?
VAERS leaves rustling…
Here are some VAERS data using MedDRA keywords like "Abnormal uterine bleeding", "Menorrhagia", "Menstrual disorder", "Menstruation irregular", "Metrorrhagia", "Heavy menstrual bleeding", "Abnormal uterine bleeding" normalized by age stratified CDC dose 1 data (the number of people who had at least 1 dose).
25-44 year olds again getting the blood end of the stick.
Here’s some VAERS data using MedDRA keywords like "Heparin", "Thrombin", "Von Willebrand", "Fibrinogen", "Plasminogen" and "Plasmin" normalized by age stratified CDC dose 1 data (the number of people who had at least 1 dose). 16 reports of heparin-related adverse events per 100,000 injections in individuals 75 years and older, is a lot of reports. Don’t forget, no URF here.
When I looked only for “Heparin” and normalized, it became clear that there is a trend toward the elderly receiving heparin.
Deep vein thromboses are happening across all ages but primarily in individuals older than 40.
I will be updating this article.
Heparin molecular mimicry - as a side note
There a paper entitled “Heparin-Mimicking Polymers: Synthesis and Biological Applications” published in 2016 that explores heparin-mimicking polymers and the implications and applications for biology. There are many applications for heparin mimickers including graphene-oxide doped heparin-mimetic hydrogels. The paper states that “heparin-mimicking polymers typically resist degradation/desulfation by heparinases” and this is quite scary considering that S1 is linked to heparin.
I thought it was interesting that Suramin is a molecular mimicker of heparin.
Paluck SJ, Nguyen TH, Maynard HD. Heparin-Mimicking Polymers: Synthesis and Biological Applications. Biomacromolecules. 2016 Nov 14;17(11):3417-3440. doi: 10.1021/acs.biomac.6b01147. Epub 2016 Oct 14. PMID: 27739666; PMCID: PMC5111123.
Heparin has traditionally been extracted from cattle lungs or pig intestines. Since concerns emerged over mad cow disease in the 1980s, cattle in most countries have been banned as a source of heparin. No synthetic heparin is on the market.
https://en.wiktionary.org/wiki/hepatic
Muñoz EM, Linhardt RJ. Heparin-binding domains in vascular biology. Arterioscler Thromb Vasc Biol. 2004 Sep;24(9):1549-57. doi: 10.1161/01.ATV.0000137189.22999.3f. Epub 2004 Jul 1. PMID: 15231514; PMCID: PMC4114236.
Eisenberg D, Jucker M. The amyloid state of proteins in human diseases. Cell. 2012 Mar 16;148(6):1188-203. doi: 10.1016/j.cell.2012.02.022. PMID: 22424229; PMCID: PMC3353745.
Idrees D, Kumar V. SARS-CoV-2 spike protein interactions with amyloidogenic proteins: Potential clues to neurodegeneration. Biochem Biophys Res Commun. 2021 May 21;554:94-98. doi: 10.1016/j.bbrc.2021.03.100. Epub 2021 Mar 24. PMID: 33789211; PMCID: PMC7988450.
Zoe Swank, Yasmeen Senussi, Galit Alter, David R. Walt. Persistent circulating SARS-CoV-2 spike is associated with post-acute COVID-19 sequelae. medRxiv 2022.06.14.22276401; doi: https://doi.org/10.1101/2022.06.14.22276401.
Letarov, A. V., Babenko, V. V., & Kulikov, E. E. (2021). Free SARS-CoV-2 Spike Protein S1 Particles May Play a Role in the Pathogenesis of COVID-19 Infection. Biochemistry. Biokhimiia, 86(3), 257–261. https://doi.org/10.1134/S0006297921030032.
Ogata AF, Cheng CA, Desjardins M, Senussi Y, Sherman AC, Powell M, Novack L, Von S, Li X, Baden LR, Walt DR. Circulating Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Vaccine Antigen Detected in the Plasma of mRNA-1273 Vaccine Recipients. Clin Infect Dis. 2022 Mar 1;74(4):715-718. doi: 10.1093/cid/ciab465. PMID: 34015087; PMCID: PMC8241425.
https://en.wikipedia.org/wiki/Antithrombin
Rudd TR, Preston MD, Yates EA. The nature of the conserved basic amino acid sequences found among 437 heparin binding proteins determined by network analysis. Mol Biosyst. 2017;13(5):852-865. doi:10.1039/c6mb00857g.







Yesterday I spent 3 hours listening to new interviews with Mike Yeadon and Geert Vanden Bossche. This morning I spent another 90 minutes listening to the new interview with Ryan Cole at mercola.com and now Jessica hits me with this. Naomi Wolf is right; we are witnessing a genocide. And the mayor of NYC has issued a jab mandate for all children this fall. And Zev Zelenko has gone to heaven. We need some good news. At least I am not jabbed! Happy 4th!
Dear Dr. Rose,
I didn't understand much of the sciency stuff presented here, but even I can tell it is NOT GOOD. What did STICK with me was:
* 25-44 year olds again getting the blood end of the stick.
* ...it became clear that there is a trend toward the elderly receiving heparin.
My mom was diagnosed in her 70s (I think) with "idiopathic thrombocytopenia" among other amorphous assignments. Sadly, she isn't here on Earth to confirm.
Could heparin adminstration have caused the "idiopathic" part? She was injected with and swallowed so much prescription stuff over the years! If she were still alive, she'd probably be first in line at the funeral home -- er, assisted care home -- for her COVID-19 jab.
Mom's "very thorough" geriatrician had her on so many meds, none of which made her feel better as far as I could tell. My trusting doctors-are-next-to-God Mom died sick and in pain, no doubt due to the great "treatment" and "care" she received. And that was years before the current COVIDera.
Bottom line: This spike protein is a bioweapon 🔪 of unspeakable 🙊 evil 😈. We must stop 🛑 these 🤼 people!