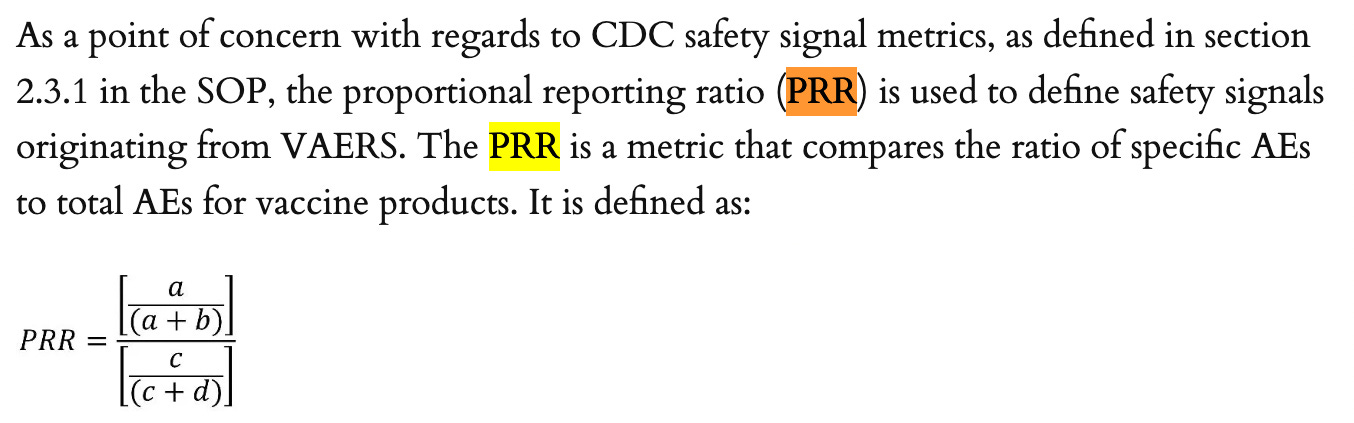
And once again, one more peek into that new ICAN data.
The chart below comes from here in the folder named: Weekly PRR Tables 3-5 May 20 2022; in the file: Table5 PRR of PTs for COVID19 mRNA Compared to 2009_2022 NON-COVID19_05.20.2022. The data below is for 5-11 year olds who succumbed to serious adverse events. PRR calculations were done by comparing COVID to non-COVID reports.
I am in disbelief at how high those signals are. 245.56 for Multisystem Inflammatory Syndrome (MISC) in children? This is a rare condition so why is the safety signal so high in the context of the COVID-19 shots?
According to the Boston’s Children’s Hospital:
Multisystem inflammatory syndrome in children (MIS-C), also called pediatric multi-system inflammatory syndrome temporally related to SARS CoV-2 (PMIS or PIMS-TS), is a potentially serious illness in children that appears to be a delayed, post-infectious complication of COVID-19 infection.
MIS-C has varied symptoms that affect several organs and systems in the body. Many children have symptoms resembling toxic shock syndrome or Kawasaki disease, in which the coronary arteries enlarge or form aneurysms. Also common are heart inflammation with impaired heart function and low blood pressure, rash or red eyes, and gastrointestinal symptoms. These symptoms can occur in different combinations.
It’s interesting that they mention Kawasaki disease, because it’s also in the list above with a PRR of 10.23 for the timeframe spanning December 14, 2020 through May 20, 2022. It’s also exceedingly rare (~8-67/100,000 children under 5) and usually affects children under 5.1
According to the Mayo Clinic the way to prevent MISC from COVID-19 is to get the COVID-19 shots.
In the U.S., COVID-19 vaccines are now offered to people age 6 months and older.
A vaccine can prevent you or your child from getting or spreading the COVID-19 virus. If you or your child gets COVID-19, a COVID-19 vaccine could prevent you or your child from becoming seriously ill.
Well, that’s interesting. Because based on what we KNOW, the shots increase susceptibility to SARS-CoV-2, increasing likelihood of COVID-19 and thus increasing the likelihood of MISC in 5-11 year olds. Interesting that the Mayo Clinic, to this day, is recommending these shots that are PROVEN by the CDC to be associated with MISC in 5-11 year olds as per their PRR calculation of 245.56. Just to give some perspective, a PRR > 2 indicates an association via the signal and indicative of a causative relationship that must be subsequently assessed.
So why wasn’t it? How many children got harmed as a result of this obscuration of data?
https://en.wikipedia.org/wiki/Kawasaki_disease





MISC and Kawasaki disease are diagnoses for essentially the same hyper-inflammatory (indiscriminate cell destruction by immune cells such as eosinophils, the suicide bombers of the immune system) disorder which especially affects the vasculature. Kawasaki disease is more often diagnosed in infants and children while MISC is typically diagnosed in older children, adolescents and young adults.
Stagi et al. 2015 "Severe vitamin D deficiency in patients with Kawasaki disease: a potential role in the risk to develop heart vascular abnormalities?" https://Clinical Rheumatology volume 35, pages 1865–1872 (2015) link.springer.com/article/10.1007/s10067-015-2970-6 (Paywalled) https://sci-hub.se/10.1007/s10067-015-2970-6 found that KD patients had even lower 25-hydroxyvitamin D levels than of ordinary children. While a little of this may be attributed to 25-hydroxyvitamin D being consumed during the illness, this is a brief period and the primary cause of the low 25-hydroxyvitamin D would be it being low to begin with, which means that very low 25-hydroxyvitamin D greatly raises the risk of Kawasaki disease - and so, MISC.
"The patients were 21 girls and 58 boys, average age 5.8 years. Their average 25(OH)D levels were 9.2ng/ml (23 nmol/L), while age-matched controls averaged 23.3 ng/mL (58 nmol/L). The average 25(OH)D level of the children who developed coronary artery abnormalities was just 4.9ng/ml (12.3 nmol/L)."
See discussion and further research at: https://vitamindstopscovid.info/00-evi/#4.5.
If the medical profession and immunologists were as interested in nutrition as they should be, news of this research would have spread like wildfire and within a year or two pretty much every doctor, nurse and immunologist would be aware of it, and so of the need for proper vitamin D3 supplementation to attain (it is hydroxylated primarily in the liver) much higher 25-hydroxyvitamin D levels.
There are hundreds of disease conditions where the same is true, not least sepsis and COVID-19. Even today, most medical professionals - and many in the health freedom movement - do not yet appreciate that proper vitamin D3 supplementation is necessary for almost everyone, since this is the only safe, practical way of attaining the 50 ng/mL (125 nmol/L = 1 part in 20,000,000 by mass) circulating 25-hydroxyvitamin D our immune systems need to function properly, all year round. There's very little vitamin D3 in food and, while UV-B exposure of ideally white skin can produce plenty of it, this is not available all year round far from the equator - and it always damages DNA and so raise the risk of skin cancer.
No matter what food we eat or lifestyle choices we make (except for high levels of ultraviolet B exposure of ideally white skin), the only way we can attain sufficient 25-hydroxyvitamin D is by supplementing proper amounts of vitamin D3 (or, in principle 25-hydroxyvitamin D) according to body weight and obesity status. The one exception is infants who are substantially breast fed by 25-hydroxyvitamin D replete mothers. Such breast milk contains both vitamin D3 and 25-hydroxyvitamin D (Tsugawa et al. 2021 https:// www.mdpi.com/2072-6643/13/2/573), the latter being more important since it is absorbed directly into the infant's circulation, while only (very approximately) 1/4 of ingested vitamin D3 is hydroxylated in the liver to circulating 25-hydroxyvitamin D.
Neither vitamin D3 cholecalciferol nor 25-hydroxyvitamin D calcifediol, made from vitamin D3, primarily in the liver) are hormones.
Please see the research cited and discussed at: https:// vitamindstopscovid.info/00-evi/. This begins with recommendations from New Jersey based Professor of Medicine, Sunil Wimalawansa on the average daily supplemental intake quantities of vitamin D3 which will attain least 50 ng/mL circulating 25-hydroxyvitamin D, over several months, without the need for blood tests or medical monitoring:
70 to 90 IU / kg body weight for those not suffering from obesity (BMI < 30).
100 to 130 IU / kg body weight for obesity I & II (BMI 30 to 39).
140 to 180 IU / kg body weight for obesity III (BMI > 39).
This is because obesity reduces the rate of hydroxylation in the liver and because the resultant 25-hydroxyvitamin D (and probably vitamin D3 itself) is sequestered in the excess adipose tissue: https://5nn.info/temp/250hd-obesity/.
For 70 kg (154 lb) body weight without obesity, this is about 0.125 milligrams (125 micrograms 5000 IU) a day. This takes several months to attain the desired > 50 ng/mL circulating 25-hydroxyvitamin D. This is 8 or more times what most governments recommend. "5000 IU" a day sounds like a lot, but it is a gram every 22 years - and pharma-grade vitamin D costs about USD$2.50 a gram ex-factory.
These recommendations are included in a recent article with another professor of medicine Scott T. Weiss and professor of pediatrics Bruce W. Hollis: https:// www.mdpi.com/2072-6643/16/22/3969. All three have been researching vitamin D for decades.
A fully functional immune system protects against cancer, autism, many chronic conditions such as auto-immune inflammatory diseases, preeclampsia, pre-term birth, sepsis and the later development of autism, ADHD, intellectual disability and schizophrenia in children and against neurodegeneration AKA dementia..
What was it, avarice , depopulation or hate for the human race ? It was NOT ignorance.