Determinants of COVID-19 Vaccine-Induced Myocarditis Requiring Hospitalization
Jessica Rose, PhD and Peter McCullough, MD
Please cite as: Rose, Jessica, & McCullough, Peter. (2022). Determinants of COVID-19 Vaccine-Induced Myocarditis Requiring Hospitalization. https://doi.org/10.5281/zenodo.6556390
Funding source(s): None related
Conflict of interest: Nothing to disclose
Abstract
Objective: To characterize determinants of COVID-19 vaccine-induced myocarditis requiring hospitalization in Vaccine Adverse Event Reporting System (VAERS) domestic data.
Design: Cross sectional, descriptive analysis of VAERS reports of COVID-19 vaccine-induced myocarditis requiring hospitalization in individuals aged 3 months to 98 years of age.
Participants: All individuals who submitted an adverse event (AE) report to VAERS associated with a diagnosis of myocarditis from December 14, 2020 through March 18, 2022.
Results: 3569/3594 (99.3%) cases of COVID-19 vaccine-induced myocarditis requiring hospitalization reports analyzed in the VAERS domestic data set were not co-associated with COVID-19 respiratory illness in accordance with either ‘negative’ polymerase chain reactions (PCR) to detect SARS-CoV-2, COVID-19 diagnosis, or both. Rates of hospitalization were high with 84% of all myocarditis reports associated with hospitalization in the 0-19 age group and 70.9, in general. Myocarditis in the context of co-presentation of elevated cardiac troponin (cTn), chest pain (CP), abnormal cardiac imaging , electrocardiogram ST segment elevation (STE) and abnormal C-reactive protein levels (CRP) was reported in the context of hospitalization in 92.2%, 85.5%, 93.5%, 93.9% and 90.3%, respectively, in children ages 0-19. 79% of all myocarditis requiring hospitalization reports were made within 7 days of injection and 48% were reported within 48 hours of injection. 90% of all myocarditis requiring hospitalization reports and 58% of reports were filed within 7 days and 48 hours, respectively in children ages 0-19. Higher reporting rates of troponin elevation, ST segment elevation and CRP abnormalities were found in 12-18-year-olds when compared to the next highest rates found in 19-29-year-olds (chi-sq; p = 0.00000000; p = 0.00000000; p = 0.00000006). The independent predictors of hospitalization were as follows: male gender, OR=1.81, 95% CI 1.68-1.95, p<0.005; age (0-19 vs. 19+) OR=2.32, 95% CI 2-2.69, p<0.005; elevated troponin (12-18 vs. all other age groups), OR=4.63, 95% CI 3.59-5.99, p<0.005; an ST elevation (12-18 vs. all other age groups), OR=4.62, 95% CI 2.99-7.13, p<0.005.
Conclusions: Among those with COVID-19 vaccine-induced myocarditis, the majority were hospitalized, and the independent predictors of hospitalization were age, male gender, positive troponin, and ST-segment elevation on the ECG. Temporal proximity of reporting to injection date and significantly higher reporting rates of cardiac troponin, electrocardiogram ST segment elevation and abnormal C-reactive proteins in young individuals (12-18) in the context of myocarditis requiring hospitalization indicate that these particular pathognomonic markers may be linked to incipient heart failure whereby the injury due to the injection is the reason for the hospitalization, and should always be measured and used as diagnostic markers for COVID-19 vaccine-induced myocarditis.
Keywords
SARS-CoV-2; C-reactive protein (CRP); electrocardiogram ST segment elevation (STE); cardiac imaging procedure abnormal (CI); Chest pain (CP); cardiac troponin elevation (cTnE); Adverse Events (AEs); Vaccine Adverse Event Reporting System (VAERS); COVID-19; myocarditis
1. Background
1.1 COVID-19 vaccine-induced myocarditis
COVID-19 injectable biological product use is prompting above-background reporting of myocarditis into many adverse event data collection systems including the Vaccine Adverse Events Reports System of the United States, and many case reports of COVID-19 vaccine-induced myocarditis have been reported. [1-33] Myocarditis is inflammation of the myocardium, or musculature, of the heart in the absence of ischemia (reduced blood flow and oxygen). [34-40][1] Although the etiology associated with myocarditis is typically viral, it can be the result of exposure to toxic substances or immune-mediated. [36] Damaged muscle is prone to lethal cardiac arrythmias as well as having the potential to develop both right and left ventricular dysfunction (cardiomyopathy), thus it is vital to diagnose early and medically intervene, if necessary. Diagnosis is commonly done by an assessment of cardiac markers and tests. [37-55]
Pre-COVID-19, background rates indicated that 1 in 100,000 children per year were affected by myocarditis and it has been reported that 0.05% of all pediatric hospitalizations are for myocarditis. [43,46,47] Arolia and colleagues found in that[JR1] the rate of myocarditis pre-COVID-19 was 4 cases/million/year among children and adolescents. Between 0.5 and 3.5% of heart failure hospitalizations are due to myocarditis. Most cases of myocarditis are identified in young adults with males affected more often than females. [41] “Data on all NHS England hospital admissions due to myocarditis between 1998 and 2017 showed that over the 19-year period there were 12,927 admissions with a primary diagnosis of myocarditis accounting for 0.04% (36.5 per 100,000) of all NHS admissions (although this condition is likely underdiagnosed).” [41]
Since the mass administration of the Pfizer Inc./BioNTech BNT162b2, Moderna mRNA-1273 and Janssen Ad26.COV2.S COVID-19 injectable biological products, only two have received biological licensing agreements but are not fully approved: COMIRNATY product (Pfizer Inc./BioNTech) and the Moderna product. FDA Biological licensing agreement letters call for more studies on COVID-19 vaccine-induced myocarditis (August 23rd, 2021) [56,57,58]. It is vital to actively monitor potential cases of COVID-19 vaccine-induced myocarditis, especially in children, and to investigate the determinants and outcomes.[2],[3] [59-88]
1.2 Vaccine Adverse Event Reporting System (VAERS)
VAERS was created in 1990 by the Food and Drug Administration (FDA) and Centers for Disease Control and Prevention (CDC) to receive reports of AEs that may be associated with vaccines. [89,90,91,92] The primary purpose for maintaining the database is to serve as an early warning or signaling system for adverse events not detected during pre-market testing and clinical trials. In spite of the fact that the National Childhood Vaccine Injury Act of 1986 (NCVIA) requires health care providers and vaccine manufacturers to report to the DHHS specific AEs following the administration of vaccines outlined in the Act,[4] under-reporting is a known imperfection of the VAERS system. [93,94,95,96,97]
A serious or severe adverse event (SAE) is defined an adverse event that can result in a life-threatening illness, death or prolonged hospitalization or incapacity.[5] [91] Myocarditis qualifies as an SAE as it is often associated with hospitalization in young individuals [98] and can be life threatening. Myocarditis requiring hospitalization is the focus of this descriptive analysis.
1.3 Background myocarditis rates and VAERS-reported myocarditis rates
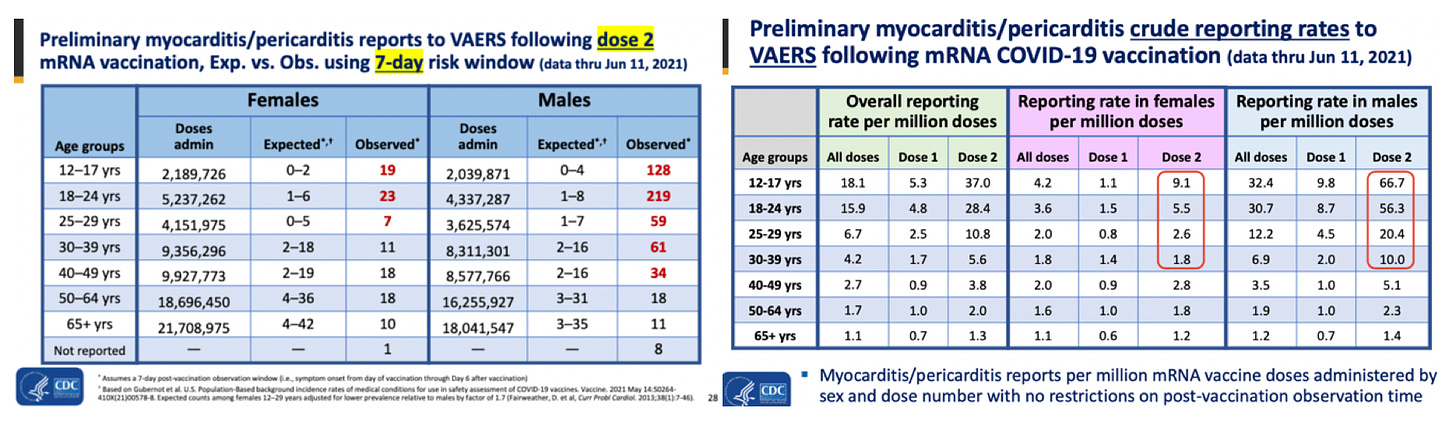
Recent published findings provide clinical evidence of COVID-19 vaccine-induced myocarditis. A study published online in the Journal of American Medical Association (JAMA) reviewed 2,000,287 electronic medical records (EMR) from 40 hospitals in the U.S. of people who received at least one dose of the COVID-19 biological products. [12] They report 20 individuals succumbed to myocarditis (1/100,000) and 37 to pericarditis (1.8/100,000) and this was linked to age: the elderly were reported to succumb to pericarditis more frequently. Importantly, they examined myocarditis and pericarditis rates for a pre-injection period spanning ~1 year starting January 2019 and they found a 62% increase in myocarditis reports and 60% increase in pericarditis reports. A COVID-19 vaccine safety update by the Advisory Committee on Immunization Practices (ACIP) (June 23rd, 2021) by Tom Shimabukuro (Supplementary Table 1), showed increased myocarditis and pericarditis reporting rates in VAERS. [97] To be clear, they reported that 66.7/1,000,000 children between the ages of 12 to 17 succumbed to myocarditis and reported to VAERS. This is up to and including June 11th, 2021 - the roll out for children aged 12-15 began on May 18th, 2021: 24 days. Thus, since administration of the COVID-19 vaccines to children aged 16 and 17 began slightly earlier, these products had been administered to children aged 12-17 for approximately 6 weeks. This means that one would expect 580/1,000,000 children per year between the ages of 12 to 17 to succumb to myocarditis as a result of the injections. 1/100,000 children are thought to suffer myocarditis each year thus 10 per million would be expected to occur in any average per year.[6] This means that the reports (ie: the reports we know of made by the CDC for the ~6-week period of roll out in to 12-17-year-olds) are 58x higher than the expected baseline rate. These estimates are likely gross underestimates since not all recipients are screened with re-exam, ECG and troponin. Supplementary Table 1 (right) also reveals a discrepancy between Dose and Dose 2 rates in both females and males. This will be addressed in the section on CausationCumulative Dose Effect.
VAERS reports following the first or second dose of the COVID-19 vaccines have previously revealed that myocarditis rates are significantly higher in youths between the ages of 13 to 23 (p<0.0001) with 86% occurring in males. [97] VAERS data also revealed 19 times the expected number of myocarditis cases in the vaccination volunteers aged 12-15 years over background myocarditis rates for this age group. [96]
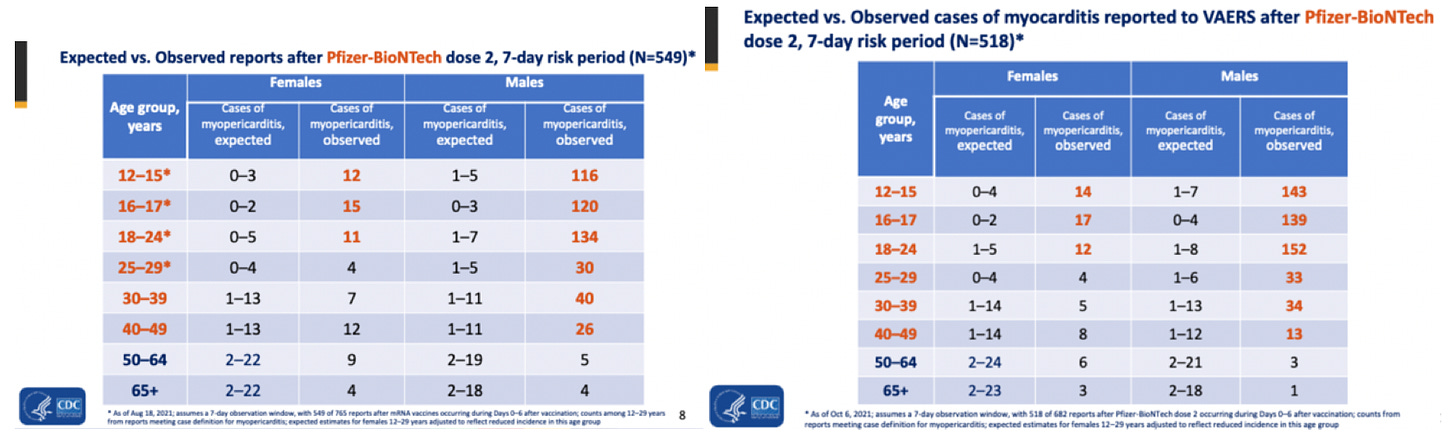
More recent evidence (Supplementary Table 2) of above background reporting rates of myocarditis in VAERS is from ACIP in 2 reports presented on August 30th and October 21st, 2021 by CDC’s John R. Su both entitled “Myopericarditis following COVID-19 vaccination: Updates from the Vaccine Adverse Event Reporting System (VAERS)”. It is striking that both reports reveal more than 100 times above-background reporting rate for males in the 12-15 age group.[7] Considering these data, and the clear above-background safety signals projected, the continuance of the COVID-19 injectable product roll-out into young children and the push to inject even younger age groups is, questionable.
1.1 Pathognomonic markers associated with myocarditis requiring hospitalization
Correct and early diagnosis is vital to minimize damage induced from COVID-19 vaccine-induced myocarditis and to maximize the medical management of myocarditis regardless of the etiology. [36,39] The clinical picture of cardiac injuries associated with the COVID-19 injections are characterized by extreme elevations in cardiac troponin levels (with cutoff 0.04 ng/mL) [42,76,77,82], chest pain and abnormal cardiac imaging, electrocardiogram readings, echocardiogram readings[8], C-reactive protein levels and cardiac magnetic resonance imaging. In addition to atypical profiles with regard to these markers, in many cases, individuals report their injuries in temporal proximity to injection. For example, both can be defined in terms of subclinical possible myocarditis (no cardiac symptoms with abnormal ECG, echocardiogram, or troponin findings consistent with myocarditis) or probable myocarditis (no cardiac symptoms without abnormal ECG, echocardiogram, or troponin findings and only abnormal CMR imaging findings) or clinical (cardiac symptoms present before or at the time of cardiac testing).[9] But, COVID-19 vaccine-induced myocarditis will be associated with an additional temporal association with COVID-19 mRNA or adenoviral DNA injections and massive troponin elevations in the absence of another known cause, for example. COVID-19 vaccine-induced myocarditis has been reported to present with clinical symptoms such as chest pain (and effort intolerance), excessively elevated cardiac troponin levels, electrocardiogram ST segment elevation, and in some cases, left and right ventricular dysfunction on echocardiography (cardiac imaging) and C-reactive protein abnormalities.[10] The emergence of COVID-19 vaccine-induced myocarditis clinical symptoms is also supported by preclinical studies and CMRI studies that recently reported myocardial damage suggestive of ‘autoimmune’ myocarditis that further distinguishes between acute inflammatory processes.
2. Methods
To analyse the VAERS data, the Language and Environment for Statistical Computing, R was used. VAERS data is available for download[11] in three separate comma-separated values (csv) files representing i) general data for each report; ii) the reported AEs or ‘symptoms’, and iii) vaccine data including vaccine manufacturer and lot number, for each report. VAERS data is updated weekly. Upon report of (an) adverse event(s), a VAERS ID number is provided to preserve confidentiality, and a detailed description of the AEs are transcribed along with the individual’s age, residence by state, past medical history, allergies and gender and many other demographic details. In addition, the vaccine lot number, place of vaccination and manufacturer details are meant to be included in the report.
In order to optimize the input variables for analysis, the three files were merged according to VAERS ID: a linking variable present in all three files. The merged data set comprises data collected pertaining to all VAERS reported AEs associated with BNT162b2, mRNA-1273, and Ad26.COV2.S products.
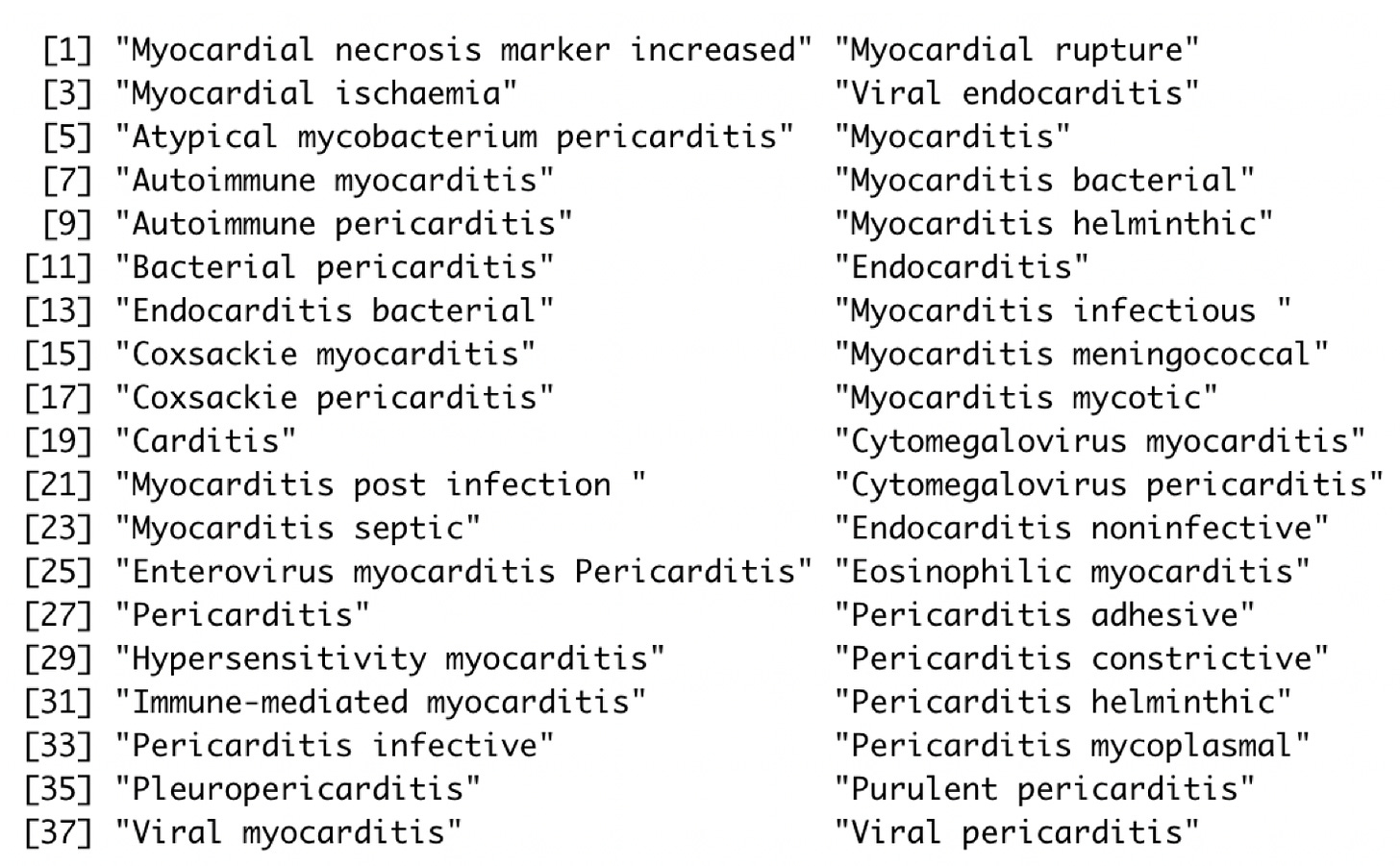
The merged data set was sorted according to vaccine type (data reported only in the context of COVID-19 products) and relevant variables were sorted according to ascending VAERS ID. A data subset including only reports of myocarditis was created by keyword search according to MedDRA nomenclature.[12],[13] Supplementary Table 1 shows the MedDRA codes used as key words.[14] [92] The myocarditis data subset was filtered to only include hospital-associated cases (myocarditis requiring hospitalization includes only reports where hospitalization was indicated (HOSPITAL == “Y”). Diagnostic markers for clinical (as opposed to subclinical) myocarditis including troponin Increases (cTnE), chest pain (CP), cardiac imaging procedure abnormal (CI), electrocardiogram ST segment elevation (STE) and abnormal C-reactive protein (CRP) levels were isolated and compared in the context of the myocarditis reports using age and gender stratification.
Statistical analysis was done using the Student’s t-Test to determine statistically significant differences between mean ages and the Chi-square test for independence was used to determine significance between categorical variables (male/female, for example). Skewing in distribution of data was tested using Pearson's Skewness Index, I, which is defined as I = (mean-mode)/standard deviation. The data set is significantly skewed if |I|≥1.
3. Results
3.1 General information
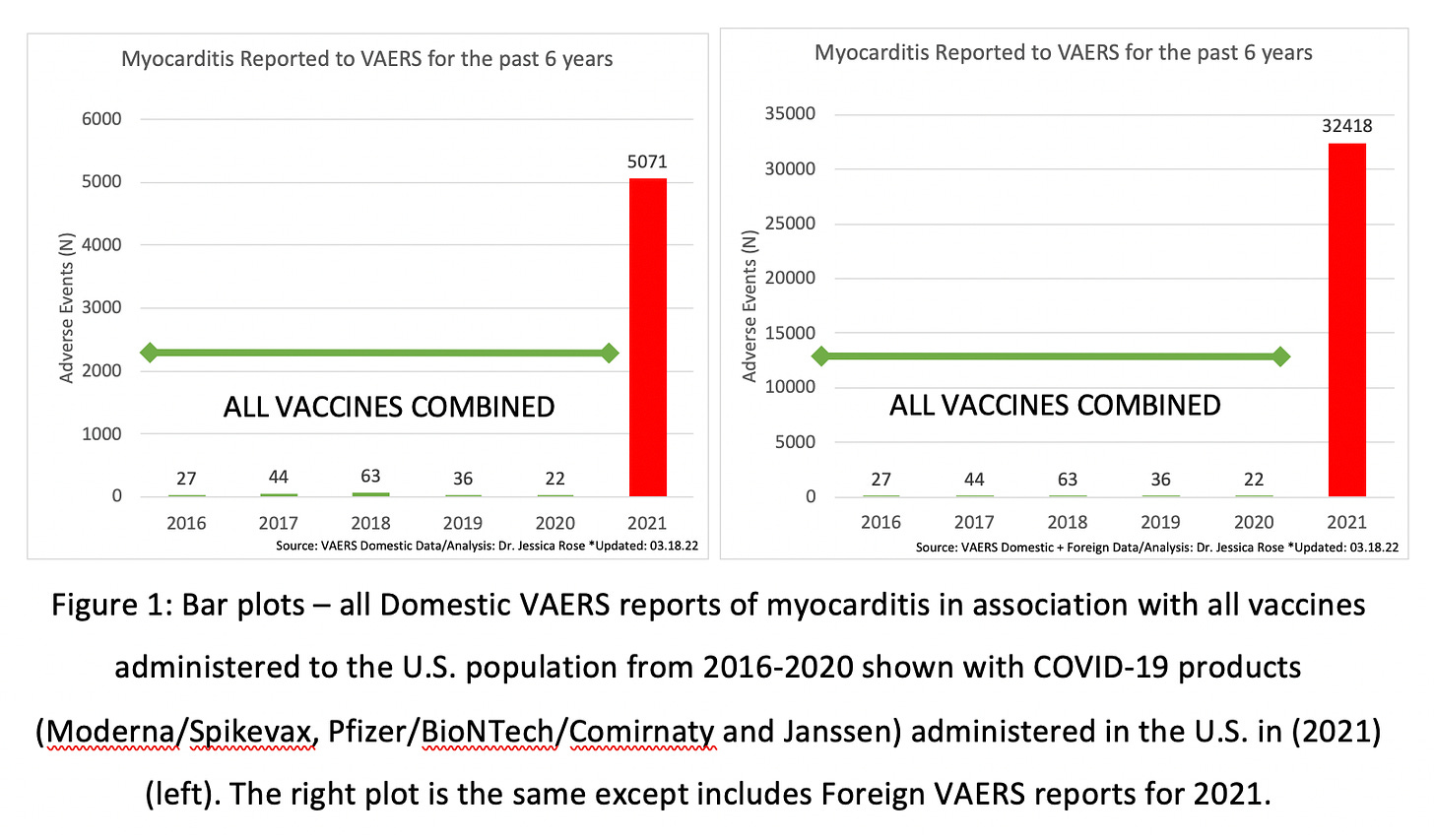
To date (March 18, 2022), approximately 5.1 billion people worldwide have received at least one dose of the COVID-19 products, including the Pfizer Inc./BioNTech BNT162b2, Moderna mRNA-1273 and Janssen Ad26.COV2.S products, with 77% of the total population of the United States having received at least one dose.[15],[16] As of March 18th, 2022, 1,099,183 AEs have been reported to the VAERS system in the context of the COVID-19 products where 753,460 AEs are from the VAERS Domestic data set. These numbers are extraordinarily atypical in comparison to total AE reports to VAERS for the past 10 years for all vaccines combined: the increase in total reports for 2021 is more than 1800%. Even more atypical, are the numbers of myocarditis reports in the context of the COVID-19 products with a more than 13,000% increase in reports as compared to the past 5 years of death data in VAERS. Figure 1 shows the total AE counts and total VAERS-reported myocarditis counts per year for the past 5 years up to and including the VAERS update on March 18th, 2021. Both the absolute numbers of total AEs and those of myocarditis per year dramatically outnumber the absolute numbers recorded in previous years. To date, there are 5,071 (<1% of all AEs) reports of myocarditis in the VAERS Domestic database and 32,418 (3%) myocarditis reports in total including the reports from the Foreign data set.
The number of cases of myocarditis reported to the VAERS database dramatically outnumber case counts seen in previous years with a 13,105% increase in reporting in the domestic data set when compared to the average number of myocarditis reports over the past 5 years. Remarkably, 5,039 (99.4%) and 10,862 (99.3%) of the reports of myocarditis to VAERS domestic and foreign data sets, respectively, are in the context of a negative PCR test for SARS-nCoV-2 and absence of COVID-19 diagnosis. (This statistic is maintained in the myocarditis requiring hospitalization group with 99.3% of reports made in the presence of negative PCR test and absence of COVID-19 diagnosis.[17]) In spite of the low COVID-19-associated rates in the context of myocarditis reports in VAERS, the COVID-19 and non-COVID-19-associated subsets of myocarditis will be compared thus creating an evidence set for characteristics of the markers specific for COVID-associated myocarditis and COVID-19 vaccine-induced myocarditis. Since myocarditis baseline rates from the United States will be compared, from this point on, only the numbers from the VAERS domestic data set will be reported.
3.2 General descriptive analysis of myocarditis reports in VAERS
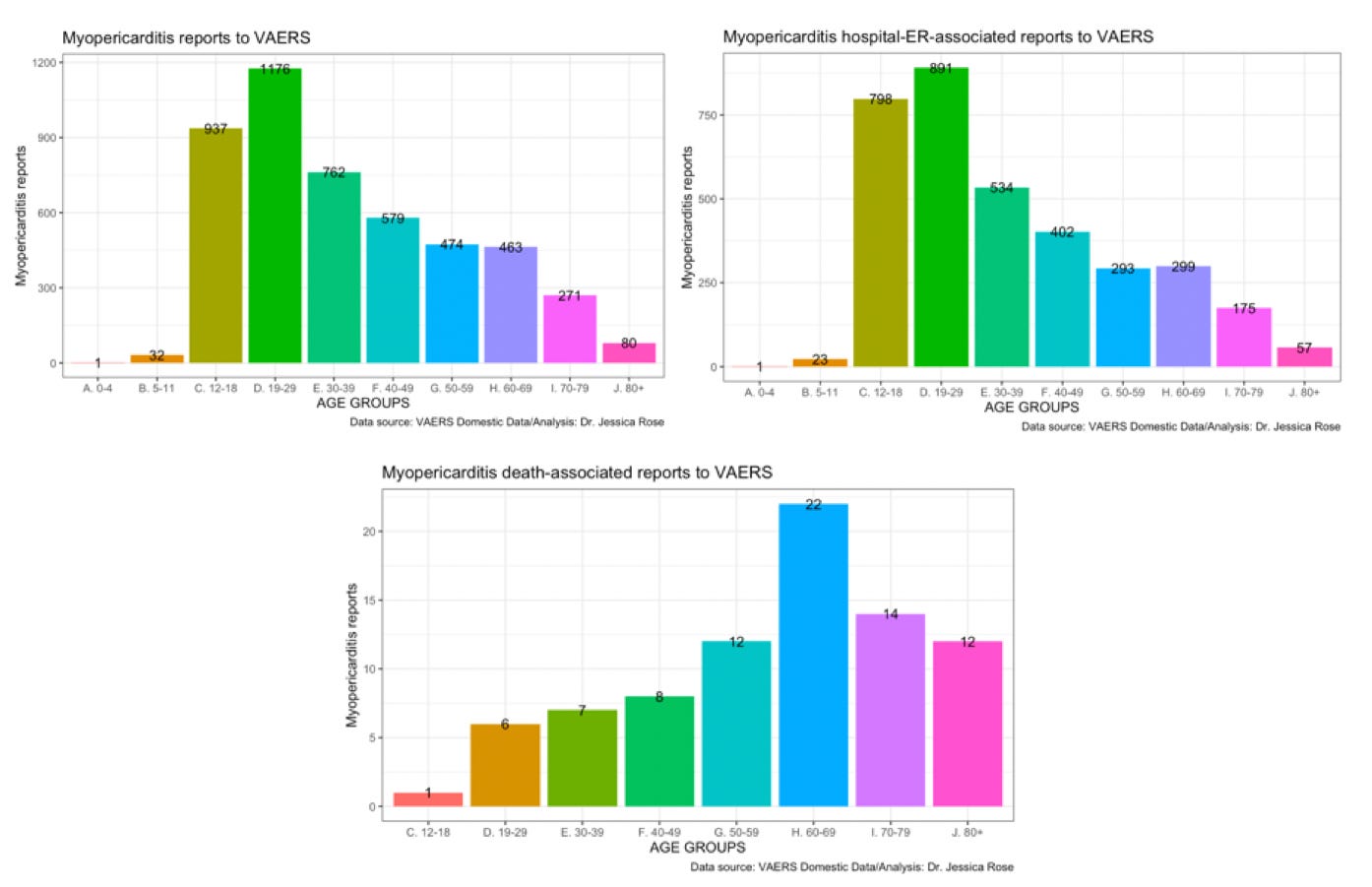
When the myocarditis dataset is age-stratified, it becomes evident that a large proportion of myocarditis reports are being made for young individuals ages 12-29 (44%) (Supplementary Figure 1). It is being repeated by public health policy members that myocarditis in young individuals is primarily ‘mild’ and ‘transient’. [10,97] However, rates of hospitalization (and emergency room visits) occur at high rates among the myocarditis reports in VAERS (70.9%) and can thus be used to rule out claims of ‘mild’ myocarditis. Interestingly, 49% of individuals hospitalized with myocarditis experienced chest pain. This and other pathognomonic markers will be discussed in the upcoming sections.
When the reports of myocarditis associated with hospitalization are stratified by age group, it becomes more obvious that young individuals are suffering at higher rates. The majority of myocarditis reports associated with death (2%) are occurring in the elderly age group 60-69. Supplementary Figure 1 also shows that half of the hospitalizations (49%) were reported in the cases of young individuals aged 12-29. One quarter (23%) of the reports were made for children aged 12-18. Subdivision of the analysis by age group follows in the upcoming section.
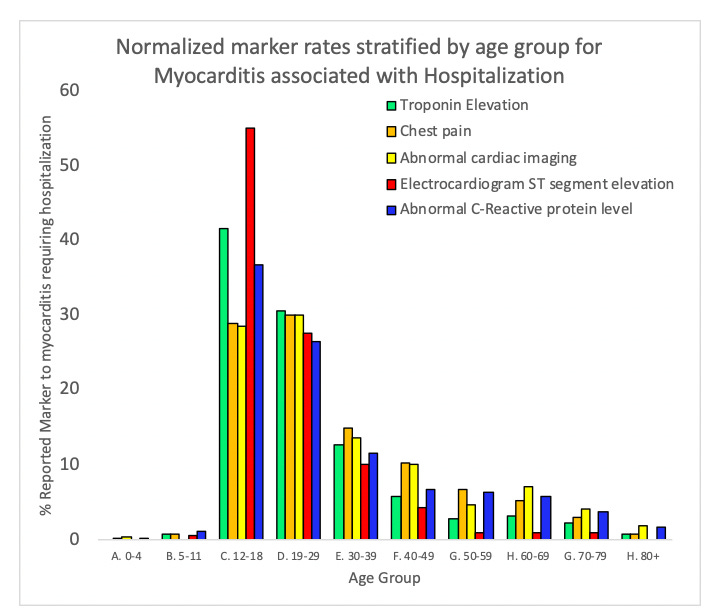
3.3 Characterizing pathognomonic markers for COVID-19 vaccine-induced myocarditis
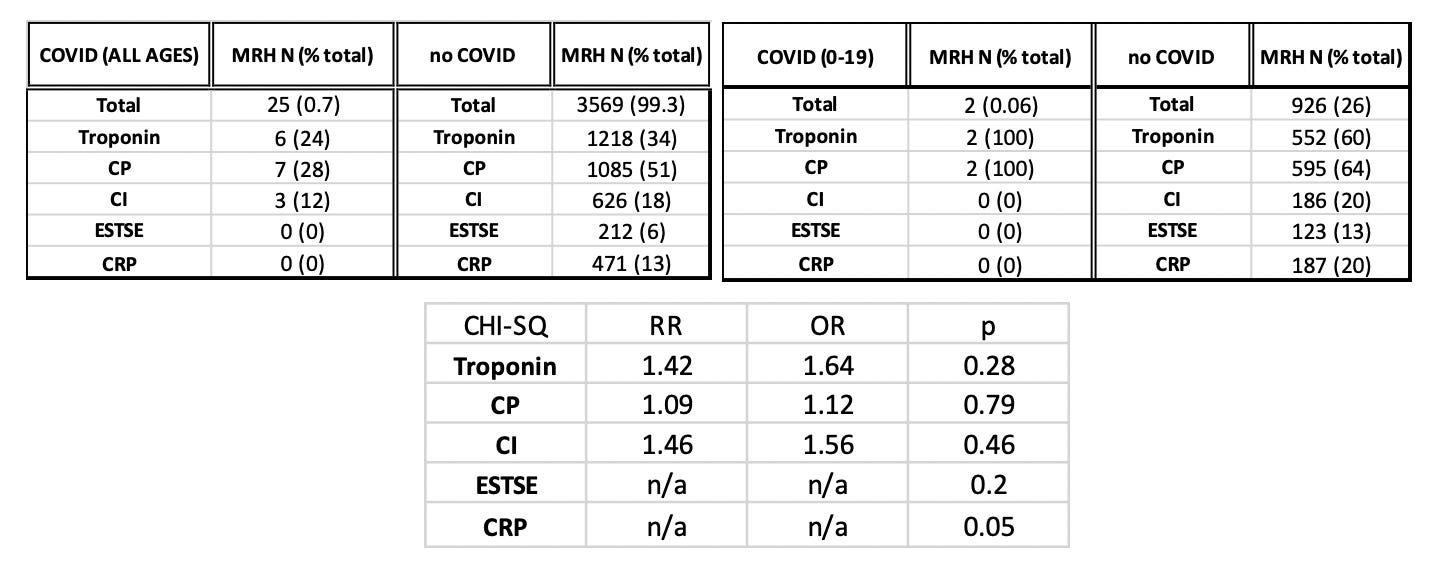
Selected clinical features of myocarditis were filtered out of the total myocarditis requiring hospitalization cases by MedDRA code. As shown in Figure 2, 70.9% of reports of myocarditis are hospital-associated. Of these, 34.1% are associated with cTnE, 50.4% are associated with CP, 17.5% are associated with abnormal CI, 5.9% are associated with STE and 13.1% are associated with abnormal CRP levels.

As previously reported, 70.9% percent of myocarditis reports are associated with hospitalization and 1.99% are associated with death (not shown). For children ages 0-19, 84% of myocarditis cases are hospital-associated with 59.7%, 64.3%, 20.0%, 13.3% and 20.2% co-associated with cTnE, CP, CI, STE and CRP, respectively. This means that there is a high preponderance of elevated troponin and chest pain with myocarditis requiring hospitalization, in general, and this preponderance is higher in younger ages. These myocarditis requiring hospitalization cases are not associated with COVID-19.
The markers in the context of the myocarditis reports were age-stratified and plotted to determine if there are preponderances of these markers in young people (Figure 2). As previously reported, 47% of myocarditis requiring hospitalization cases are made in the context of young individuals ages 12-29 (Figure 3). Of these reports, 50% were associated with troponin elevation, 62% cChest pain, 14% abnormal cardiac imaging, 10% electrocardiogram ST segment elevation 17% C-reactive protein (Supplementary Figure 2). [18]
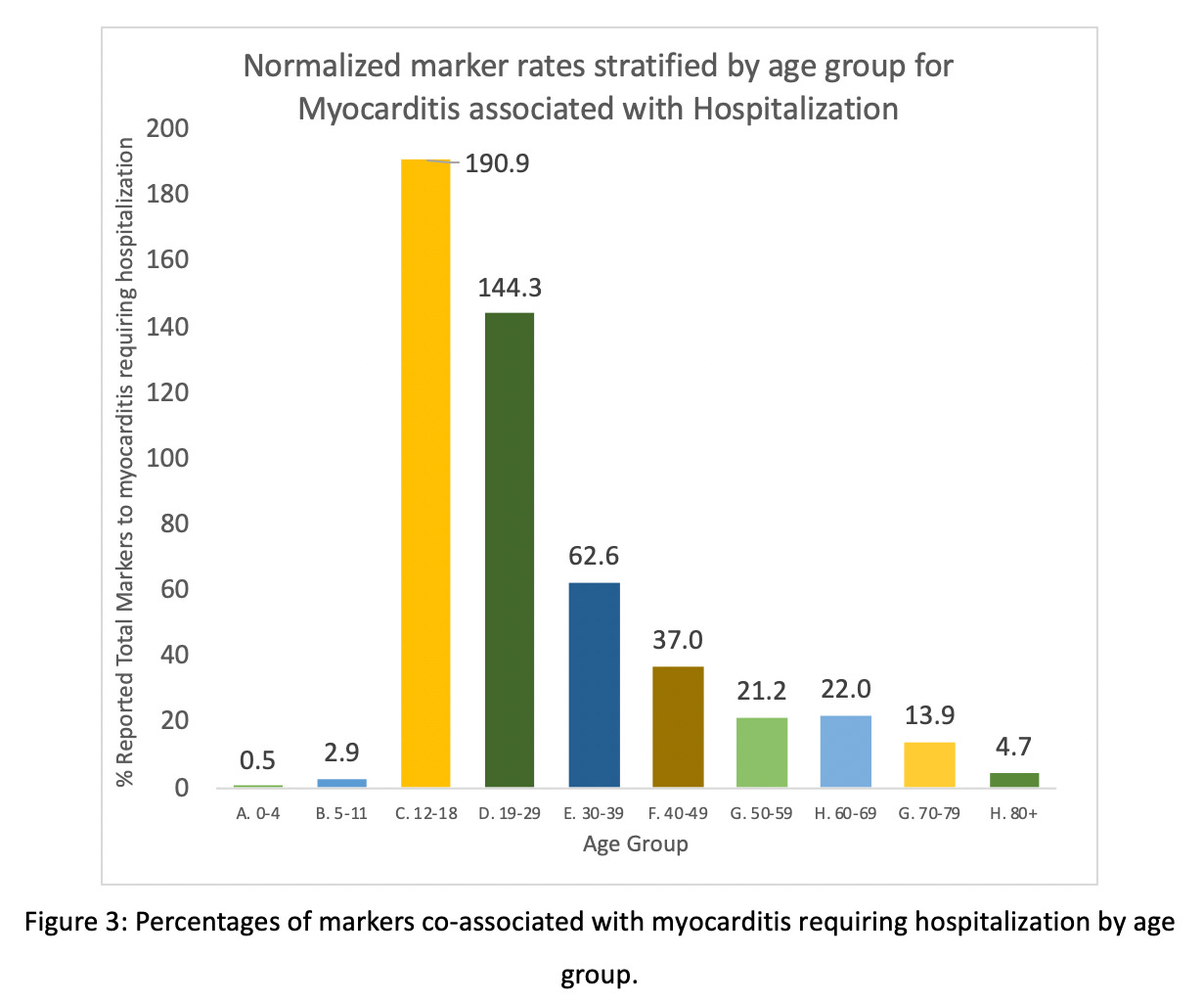
If only the younger age group 12-18 is considered (this group represents 22% of all of the myocarditis requiring hospitalization reports), these percentages become 62%, 65%, 14%, 15% and 21%, for cTnE, CP, CI, STE and CRP, respectively. Thus, even in the small range of ages in the 12-18 age group, approximately half of the reports are associated with elevated troponin and ECG ST segment elevations and one-third to one-quarter are associated with abnormal CRP levels, chest pain and abnormal cardiac imaging. It is interesting to note that STE is most prevalent in the 12-18-year-olds – significantly so (p =< 0.00000006) - and more prevalent than any other marker (31% higher than for the 19-29-year-olds). Troponin elevation is highest in 12-18-year-olds and is 20% higher than in the 19-29-year-old age group (p = 0.000000). CRP abnormalities are also statistically-significantly higher in 12-18-year-olds than for 19-29-year-olds (p = 0.000045) (Supplementary Table 2).
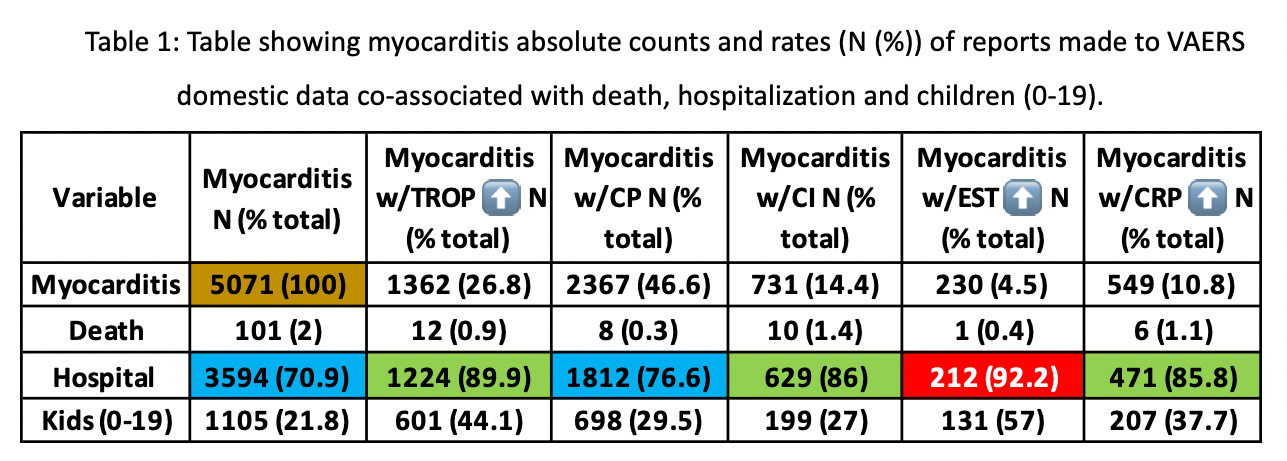
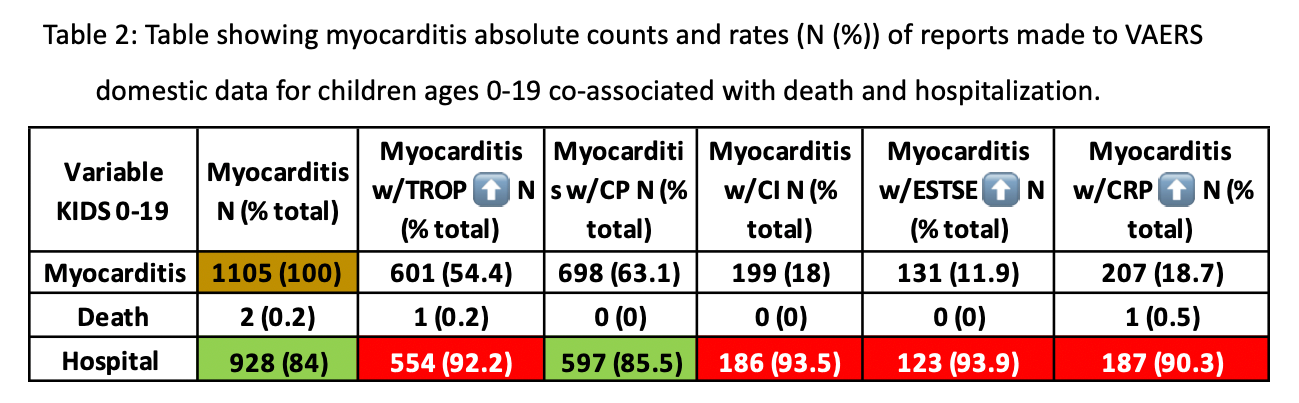
Table 1 shows a summary of the total counts for each marker in co-association with myocarditis and the percentages of the total respective variable in the context of death, hospitalization and children ages 0-19.
If one suffers myocarditis and is hospitalized, then in 89.9% of cases, troponins are elevated and in 92.2% of cases the individual has ST segment elevation. Also of note, 86% of the cases involve abnormal cardiac MRI. Children ages 0-19 represent approximately half of all cases involving elevations in troponins and EST. Boxes shaded cyan are rates that exceed 70%, boxes shaded green are rates that exceed 85% and red boxes show rates that exceed 90% meaning that 92.2% of reports of electrocardiogram ST segment elevations measured in the context of myocarditis involved hospitalization.
The rate of the vaccine-induced myocarditis requiring hospitalization becomes even clearer if the data is organized according to ambulatory versus non-ambulatory reports. The following bar plot shows the number ratio of myocarditis-associated non-ambulatory reports versus ambulatory reports. The non-ambulatory reports comprise a mere 27% of all reports.
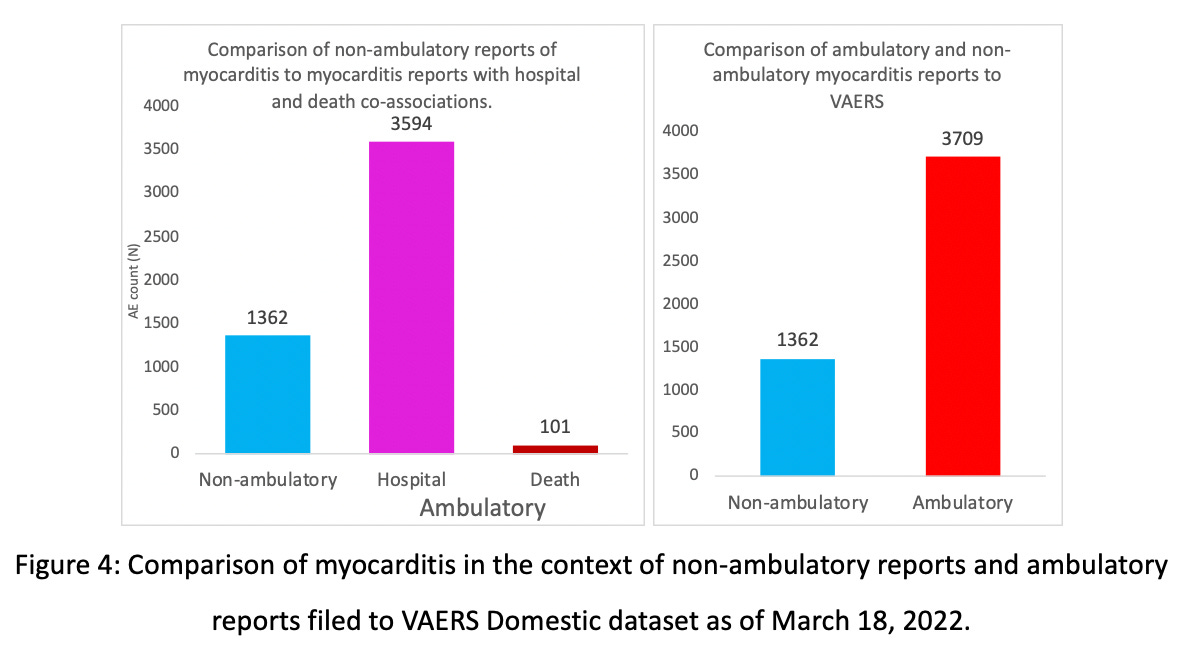
Non-ambulatory reports in the context of myocarditis (these are the reports that did not involve hospitalization), are less prominent than ambulatory reports made in this context (chi-sq. -> p=0.000). In fact, when myocarditis ensues, one is 12X more likely to be hospitalized (OR=11.89; CI=10.2-13.9; p=0.000).
Table 2 is the same as Table 1, conceptually, but includes the data for only children ages 0-19. Except for the CP clinical marker, the pathognomonic markers are reported at extremely high rates – almost exclusively with regardin the context tofo hospitalization. This means that half (54.4%) of the children aged 0-19 are reported to have elevated troponin and of those children 92.2% are hospitalized. In general, half (46.6%) of all myocarditis cases were associated with chest pain of those, 76.6% involved hospitalization.
3.4 Comparison of myocarditis requiring hospitalization in the presence and absence of COVID-19 reporting
If negative PCR tests are used as confirmation of the absence COVID-19 in the presence of myocarditis, then the resulting clinical manifestation of myocarditis must be either from a previous injury to the heart, or from the injections. When the COVID-19-associated cases are separated and compared to the non-COVID-19 cases, there is no significant difference in the deaths between the myocarditis cases associated with COVID-19, 2% vs. 3.1% for no COVID-19 versus COVID-19, respectively. There is also no significant difference between hospitalizations in COVID-19-associated myocarditis reports, 70.8% vs. 78.1% for no COVID-19 versus COVID-19, respectively. Interestingly, for myocarditis cases in children ages 0-19 without COVID-19 association, 84% involve hospitalization versus 66.7% in the case where there is a COVID-19 association. Although this difference is not statistically significant (p=0.4), this data indicates that COVID-19-associated myocarditis in children is less associated with hospitalization than COVID-19 vaccine-induced myocarditis and thus it appears as though the injections induce worse outcome with regard to myocarditis if we measure outcome by hospitalization.
Among all cases of myocarditis all ages, 32 (0.6%) had co-incident COVID-19 respiratory illness and among those 1 died and 25 (78.1) were hospitalized. Of these cases, there were 3 (9.4%) children ages 0-19 and among those none died and 2 (6.3%) were hospitalized. Among all cases of myocarditis all ages, 5039 (99.4%) had no co-incident COVID-19 respiratory illness and among those 100 (2%) died and 3069 (70.8%) were hospitalized. Of the non-co-incident COVID-19 respiratory illness cases, 1102 (22%) were 0-19 years of age. Of these children, 2 (0.2%) died and 926 (84%) were hospitalized.
When the COVID-19 versus non-COVID-19 cases of myocarditis requiring hospitalization were compared in the context of the markers, although the differences are not statistically significant except in the case of CRP (p=0.28; p=0.79; p=0.46;p=0.2;p=0.05, respectively), they are higher in all cases in the absence of COVID as shown in Supplementary Table 2.
Another way to examine the COVID-19/non-COVID-19-associated data from VAERS is to superimpose the myocarditis cases for each by age group to determine if there is an observable difference in COVID-19-association within each age group. Among all cases of myocarditis ages >19 years, 28 had co-incident COVID-19 respiratory illness and among those 23 were hospitalized and 1 died. Similarly, among all cases of myocarditis ages 0-19 years, 3 had co-incident COVID-19 respiratory illness and among those 2 were hospitalized and 0 died.
Interestingly, in children ages 12-18, there is a difference in reporting rate whereby children in this age group report higher rates of myocarditis requiring hospitalization in the absence of COVID-19. In individuals 80 years of age or older, the opposite is observed whereby the reporting rate of myocarditis requiring hospitalization is much higher in the presence of COVID-19. It should be noted that the rates of reporting on the context of COVID-19 are very low so these results are simply notable observations.
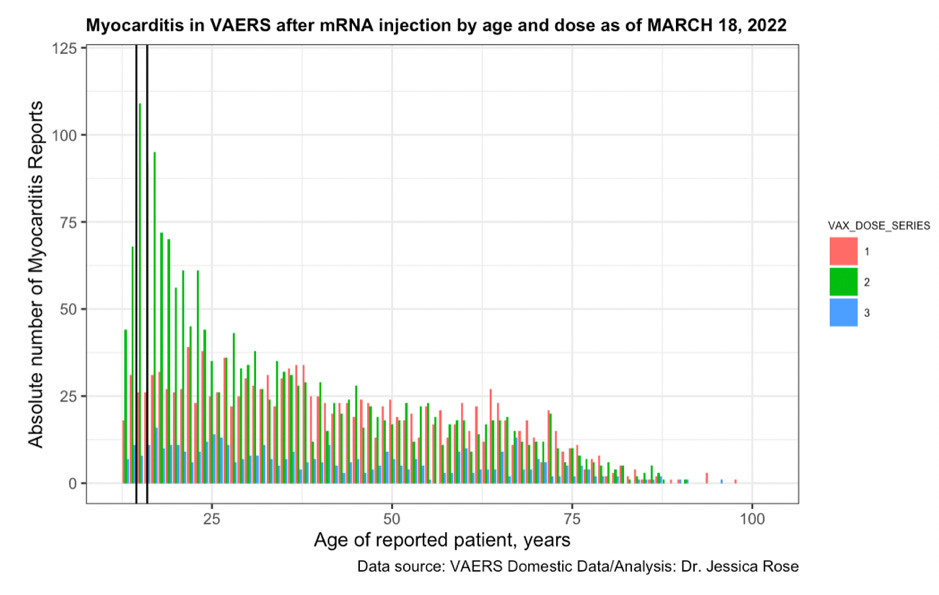
3.5 Cumulative Dose Effect
When the myocarditis reports are plotted according to age and dose (1, 2 and 3), it becomes apparent that the reporting rate has a 4-fold difference in the young following dose 2. 15-year-olds (outlined by black lines in Figure 5) are the highest reporters of myocarditis in VAERS following dose 2 and represent 11% of the total myocarditis requiring hospitalization cases. Dose 3 reporting is dramatically lower in comparison to both dose 1 and dose 2 and this is likely due to fewer individuals getting dosed a third time. There are 2.65 fewer 3rd doses than 1st doses administered as of March 18th, 2022 in the United States. This is confirmed by the CDC’s U.S. Coronavirus vaccine tracker statistics.[19] This dose response provides evidence of a causal effect of the COVID-19 vaccines and myocarditis in children.
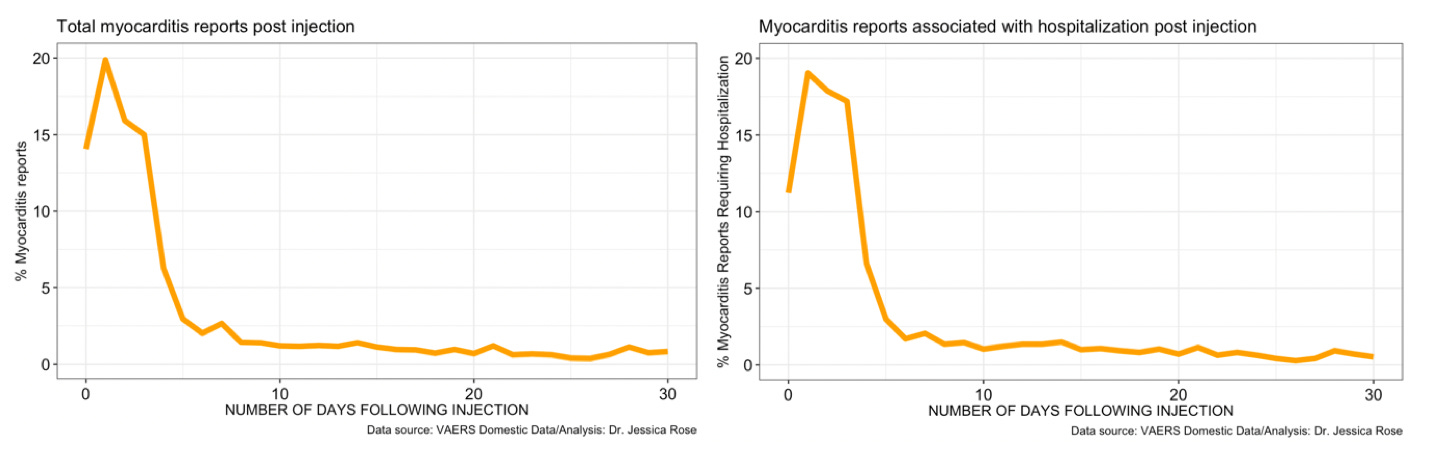
It was reported in October 2021 as part of a case study entitled “COVID-19 vaccine-induced myocarditis: Case report with literature review”, that ‘patients reported myocarditis symptoms within three days of receiving the first/second dose; however, most presentations correlated with the second dose of the COVID-19 vaccine’.[20] It is notable that 34% and 50% of total myocarditis reports (including reports of myocarditis requiring hospitalization) were filed to VAERS within 24 and 48 hours. 79% were filed within 7 days of injection. It is also notable that 30% and 48% of myocarditis requiring hospitalization reports were filed to VAERS within 24 and 48 hours. This means that within 2 days, half of all individuals had not only succumbed to myocarditis but had been diagnosed as such and successfully filed a VAERS report. 79% of myocarditis reports were filed to VAERS within the 7 days of the injections. (See Supplementary Figure 3)
4. Discussion
We found that COVID-19 vaccine-induced myocarditis was common and frequently required hospitalization. The determinants of hospitalization were older age, male gender, troponin elevation and ST-segment elevation. While rare, concurrent COVID-19 respiratory illness was more frequently related to COVID-19 vaccine- induced myocarditis in older age groups.
There is an historically unprecedented absolute number of reports of AEs in the VAERS database in the context of general AE reports. The rate of SAEs is typically 15% of the total number and has consistently (from week to week) remained at 18% for the entirety of the COVID-19 vaccine roll-out in the United States. There are also an unprecedented number of types of AEs (over 10,000 types[21], as of March 18, 2022) reported to VAERS in the context of the COVID-19 injectable biological products. Specifically, myocarditis reporting rates in VAERS are also entirely atypical with an over 13,000% increase in the reporting frequency when compared to the past 5 years of reports. This is not due to the excess number of doses administered in the United States in the context of COVID-19 vaccines. According to the CDC, 193.8 million doses of flu vaccine have been distributed in the United States as of February 26, 2021 (for the 2020-2021 flu season): “the highest number of doses in a single flu season”.[22] 558 million doses of COVID-19 vaccines were administered in the United States from December 14, 2020, through March 21, 2022. This is 462 days. A flu season is a year (365 days), thus it would be fair to assume that if 193.8 doses of flu vaccine were administered in 365 days then ~245 million doses would be administered in 462 days. Assuming that there were 2.3 times more doses of COVID product administered than for the flu for the same time period of 462 days, it would make sense then, that the rate of reporting in VAERS (for the same range of adverse events as reported for the flu) would be about twice for COVID than for flu. Twice as many doses - a proportional number of reporting - twice as many reports.
As of March 25, 2022, according to the WONDER/CDC system, there were 1,696 different types of adverse events and 45,650 total adverse events reported to VAERS in the context of the 14 variations of flu vaccines. Also according to the WONDER/CDC system, there were 10,526 different types of adverse events and 5,368,444 total adverse events reported to VAERS in the context of the 3 variations of the COVID-19 products used in the United States.[23] Thus, there are twice as many COVID shots than flu shots, 6.2 times as many types of adverse event types reported in the context of the COVID shots and 117.6 times as many reports of adverse events in the context on the COVID shots. Therefore, even though all the other vaccines were not considered in this comparison (there are 82 other types), there is no contest in this case with regard to the number of shots and the relationship to the number of AEs occurring and being reported, and the ‘anticipated’ doubling of the reports is certainly not seen as would be expected if the injection to AE ratio was proportional for flu and COVID products.
Almost half (44%) of the reports of myocarditis in VAERS are for young individuals ages 12-29 and of these, 62% were hospitalized. Children ages 0-19 comprise 22% of the myocarditis reports and of those, 69% were hospitalized. The CDC[24], FDA and other health care organizations refer to myocarditis as ‘mild’ and ‘transient’ and do not consider this serious ailment to be so in children enough to warrant a stop gap in the roll-out to prevent cases of injection-associated childhood myocarditis. “CDC continues to recommend that everyone ages 5 years and older get vaccinated for COVID-19. The known risks of COVID-19 illness and its related, possibly severe complications, such as long-term health problems, hospitalization, and even death, far outweigh the potential risks of having a rare adverse reaction to vaccination, including the possible risk of myocarditis or pericarditis.” The data from where they draw these comparisons should be made transparent. Childhood death from COVID-19 is far rarer than childhood rates of myocarditis leading to lifelong health problems according to data.
Our study has all the limitations of reports from spontaneous reported safety event databases that rely on the entry of information by the end-user, most commonly a healthcare professional (Meisner et. al Pediatrics, 2022) and later confirmation by the CDC. VAERS has inherent limitations, one being human error where column vector field entries are incomplete in the case of many VAERS ID entries. Cases (individuals) in this report may have been biased towards hospital-associated diagnoses of myocarditis, since ambulatory cases may have gone unreported. It is assumed that individuals (and their data) used in this analysis were treated equally upon hospitalization and that upon presentation of myocarditis-like symptoms, the specific markers (cTnE, CP, CI, STE, CRP) were assessed or tested, in addition to others, and a diagnosis made based on the results of these tests. Finally, we did not have external adjudication of myocarditis beyond the CDC officers who routinely call and validate cases with the reporting physician.
Unlike the majority of reports of myocarditis that follow SARS-CoV-2 respiratory infection which rely upon ICD-10 codes, our study found that COVID-19 vaccine-induced myocarditis is well characterized by clinical data supporting the actual diagnosis and that its ramifications including hospitalization of a previously well individual are serious and concerning.
5. Conclusion
COVID-19 injectable product use is prompting above-background reporting of myocarditis and pericarditis into VAERS. Recent published findings provide evidence of COVID-19 vaccine-induced myocarditis that is disparate from COVID-19-associated myocarditis. Of the 5,071 total clinically-related myocarditis AE reports in VAERS made as of March 18th, 2021, 101 individuals have died, which comprises 2% of the total myocarditis reports, 70.9% involve hospitalization and 21.8% of all cases are children aged 0-19.
COVID-19 injectable products are novel and have a genetic, pathogenic mechanism of action causing uncontrolled expression and production of SARS-CoV-2 spike protein within human cells. When you combine this fact with the temporal relationship of AE occurrence and reporting, biological plausibility of cause and effect, and the fact that these data are internally and externally consistent with emerging sources of clinical data, it supports a conclusion that the COVID-19 biological products are deterministic for the myocarditis cases observed after injection.
It would be prudent to stop all further roll-out of these product and to maintain a strict protocol for measuring the pathognomonic markers for myocarditis requiring hospitalization in individuals reporting to VAERS. [99-101]
References
1. Abbate, A., Gavin, J., Madanchi, N., Kim, C., Shah, P. R., Klein, K., Boatman, J., Roberts, C., Patel, S., & Danielides, S. (2021). Fulminant myocarditis and systemic hyperinflammation temporally associated with BNT162b2 mRNA COVID-19 vaccination in two patients. International journal of cardiology, 340, 119–121. https://doi.org/10.1016/j.ijcard.2021.08.018.
2. Abu Mouch S., et al. Myocarditis following COVID-19 mRNA vaccination. Vaccine. 2021;39(29):3790–3793. doi: 10.1016/j.vaccine.2021.05.087. PMID: 34092429; PMC8162819.
3. Albert E, Aurigemma G, Saucedo J, Gerson DS. Myocarditis following COVID-19 vaccination. Radiol Case Rep. 2021;16(8):2142-2145. doi:10.1016/j.radcr.2021.05.033.
4. Al-Rasbi, S. et al. (2022). Myocarditis, Pulmonary Hemorrhage, and Extensive Myositis with Rhabdomyolysis 12 Days After First Dose of Pfizer-BioNTech BNT162b2 mRNA COVID-19 Vaccine: A Case Report. The American journal of case reports, 23, e934399. https://doi.org/10.12659/AJCR.934399.
5. Badshah, M., Shriver, J., Rynders, B., Sjovold, A., Shaukat, M., & Rajpurohit, N. (2021). MODERNA mRNA-1273 vaccine-associated myopericarditis in a patient with a subclinical autoimmune predisposition. Journal of cardiology cases, 24(5), 227–229. https://doi.org/10.1016/j.jccase.2021.09.007.
6. Bozkurt B, Kamat I, Hotez PJ. Myocarditis With COVID-19 mRNA Vaccines. Circulation. 2021 Aug 10;144(6):471-484. doi: 10.1161/CIRCULATIONAHA.121.056135. Epub 2021 Jul 20. PMID: 34281357; PMCID: PMC8340726.
7. Can Li, et al. Intravenous injection of COVID-19 mRNA vaccine can induce acute myopericarditis in mouse model, Clinical Infectious Diseases, 2021, ciab707, https://doi.org/10.1093/cid/ciab707.
8. Chamling B, et al. Occurrence of acute infarct-like myocarditis following COVID-19 vaccination: just an accidental co-incidence or rather vaccination-associated autoimmune myocarditis? Clin Res Cardiol. 2021 Jul 31:1–5. doi: 10.1007/s00392-021-01916-w. Epub ahead of print. PMID: 34333695; PMCID: PMC8325525.
9. Chelala L, Jeudy J, Hossain R, Rosenthal G, Pietris N, White CS. Cardiac MRI Findings of Myocarditis After COVID-19 mRNA Vaccination in Adolescents. AJR Am J Roentgenol. 2022 Apr;218(4):651-657. doi: 10.2214/AJR.21.26853. Epub 2021 Oct 27. PMID: 34704459.
10. Das BB, Moskowitz WB, Taylor MB, Palmer A. Myocarditis and Pericarditis Following mRNA COVID-19 Vaccination: What Do We Know So Far? Children (Basel). 2021 Jul 18;8(7):607. doi: 10.3390/children8070607. PMID: 34356586; PMCID: PMC8305058.
11. Das BB, et al. Myopericarditis after messenger RNA Coronavirus Disease 2019 Vaccination in Adolescents 12 to 18 Years of Age. J Pediatr. 2021 Nov;238:26-32.e1. doi: 10.1016/j.jpeds.2021.07.044. Epub 2021 Jul 30. PMID: 34339728; PMCID: PMC8321962.
12. Diaz GA, Parsons GT, Gering SK, Meier AR, Hutchinson IV, Robicsek A. Myocarditis and Pericarditis After Vaccination for COVID-19. JAMA. 2021;326(12):1210–1212. doi:10.1001/jama.2021.13443.
13. Dionne, A., Sperotto, F., Chamberlain, S., Baker, A. L., Powell, A. J., Prakash, A., Castellanos, D. A., Saleeb, S. F., de Ferranti, S. D., Newburger, J. W., & Friedman, K. G. (2021). Association of Myocarditis With BNT162b2 Messenger RNA COVID-19 Vaccine in a Case Series of Children. JAMA cardiology, 6(12), 1446–1450. https://doi.org/10.1001/jamacardio.2021.3471.
14. Frustaci, A., Verardo, R., Galea, N., Lavalle, C., Bagnato, G., Scialla, R., & Chimenti, C. (2022). Hypersensitivity Myocarditis after COVID-19 mRNA Vaccination. Journal of clinical medicine, 11(6), 1660. https://doi.org/10.3390/jcm11061660.
15. Harris KM, Mackey-Bojack S, Bennett M, Nwaudo D, Duncanson E, Maron BJ. Sudden Unexpected Death Due to Myocarditis in Young People, Including Athletes. Am J Cardiol. 2021 Mar 15;143:131-134. doi: 10.1016/j.amjcard.2020.12.028. Epub 2020 Dec 19. PMID: 33347841.
16. Hudson B, Mantooth R, DeLaney M. Myocarditis and pericarditis after vaccination for COVID-19. J Am Coll Emerg Physicians Open. 2021 Jul 26;2(4):e12498. doi: 10.1002/emp2.12498. PMID: 34337595; PMCID: PMC8313036.
17. Kim HW, Jenista ER, Wendell DC, Azevedo CF, Campbell MJ, Darty SN, Parker MA, Kim RJ. Patients With Acute Myocarditis Following mRNA COVID-19 Vaccination. JAMA Cardiol. 2021 Jun 29:e212828. doi: 10.1001/jamacardio.2021.2828. Epub ahead of print. PMID: 34185046; PMCID: PMC8243258.
18. Luk A, et al. Myocarditis and Pericarditis following COVID-19 mRNA Vaccination: Practical Considerations for Care Providers. Can J Cardiol. 2021 Aug 7:S0828-282X(21)00624-3. doi: 10.1016/j.cjca.2021.08.001. Epub ahead of print. PMID: 34375696; PMCID: PMC8349442.
19. Mei R, Raschi E, Forcesi E, Diemberger I, De Ponti F, Poluzzi E. Myocarditis and pericarditis after immunization: Gaining insights through the Vaccine Adverse Event Reporting System. Int J Cardiol. 2018 Dec 15;273:183-186. doi: 10.1016/j.ijcard.2018.09.054. Epub 2018 Sep 14. PMID: 30236504.
20. Montgomery J, et al. Myocarditis Following Immunization With mRNA COVID-19 Vaccines in Members of the US Military. JAMA Cardiol. 2021 Jun 29. doi: 10.1001/jamacardio.2021.2833. Epub ahead of print. PMID: 34185045.
21. Nassar M, Nso N, Gonzalez C, et al. COVID-19 vaccine-induced myocarditis: Case report with literature review [published correction appears in Diabetes Metab Syndr. 2021 Sep-Oct;15(5):102277]. Diabetes Metab Syndr. 2021; 15(5):102205. doi:10.1016/j.dsx.2021.102205.
22. Parmar, K., Mekraksakit, P., Del Rio-Pertuz, G., Sethi, P., Motes, A., Hughes, M., Wischmeyer, J., Carbajal, L., & Sosa, E. A. (2021). Myocarditis following COVID-19 mRNA vaccination. Proceedings (Baylor University. Medical Center), 35(2), 209–213. https://doi.org/10.1080.
23. Salah HM, Mehta JL. COVID-19 Vaccine and Myocarditis. Am J Cardiol. 2021 Jul 12:S0002-9149(21)00639-1. doi: 10.1016/j.amjcard.2021.07.009. Epub ahead of print. PMID: 34399967; PMCID: PMC8272967.
24. Schauer J, et al. Persistent Cardiac MRI Findings in a Cohort of Adolescents with post COVID-19 mRNA vaccine myopericarditis, The Journal of Pediatrics (2022), doi: https:// doi.org/10.1016/j.jpeds.2022.03.032.
25. Schmitt, P., Demoulin, R., Poyet, R., Capilla, E., Rohel, G., Pons, F., Jégo, C., Sidibe, S., Druelle, A., Brocq, F. X., Dutasta, F., & Cellarier, G. R. (2021). Acute Myocarditis after COVID-19 vaccination: A case report. La Revue de medecine interne, 42(11), 797–800. https://doi.org/10.1016/j.revmed.2021.10.003.
26. Shaw KE, Cavalcante JL, Han BK, Gössl M. Possible Association Between COVID-19 Vaccine and Myocarditis: Clinical and CMR Findings. JACC Cardiovasc Imaging. 2021 Jun 16:S1936-878X(21)00485-X. doi: 10.1016/j.jcmg.2021.06.002. Epub ahead of print. PMID: 34246586; PMCID: PMC8245050.
27. Singh B, Kaur P, Cedeno L, Brahimi T, Patel P, Virk H, Shamoon F, Bikkina M. COVID-19 mRNA Vaccine and Myocarditis. Eur J Case Rep Intern Med. 2021 Jun 14;8(7):002681. doi: 10.12890/2021_002681. PMID: 34268277; PMCID: PMC8276934.
28. Truong DT, et al. Clinically Suspected Myocarditis Temporally Related to COVID-19 Vaccination in Adolescents and Young Adults. Circulation. 2021 Dec 6. doi: 10.1161/CIRCULATIONAHA.121.056583. PMID: 34865500.
29. Tsilingiris, D., Vallianou, N. G., Karampela, I., Liu, J., & Dalamaga, M. (2022). Potential implications of lipid nanoparticles in the pathogenesis of myocarditis associated with the use of mRNA vaccines against SARS-CoV-2. Metabolism open, 13, 100159. https://doi.org/10.1016/j.metop.2021.100159.
30. Vidula MK, Ambrose M, Glassberg H, Chokshi N, Chen T, Ferrari VA, Han Y. Myocarditis and Other Cardiovascular Complications of the mRNA-Based COVID-19 Vaccines. Cureus. 2021 Jun 10;13(6):e15576. doi: 10.7759/cureus.15576. PMID: 34277198; PMCID: PMC8270057.
31. Won, T., Gilotra, N. A., Wood, M. K., Hughes, D. M., Talor, M. V., Lovell, J., Milstone, A. M., Steenbergen, C., & Čiháková, D. (2022). Increased Interleukin 18-Dependent Immune Responses Are Associated With Myopericarditis After COVID-19 mRNA Vaccination. Frontiers in immunology, 13, 851620. https://doi.org/10.3389/fimmu.2022.851620.
32. Clinical considerations: myocarditis and pericarditis after receipt of mRNA COVID-19 vaccines among adolescents and young adults. 2021. https://www.cdc.gov/vaccines/covid-19/clinical-considerations/myocarditis.html [cited 2021 6/14/2021] Content source: National Center for Immunization and Respiratory Diseases.
33. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/safety/myocarditis.html
34. A. John Camm, Thomas F. Lüscher, Gerald Maurer, Patrick W. Serruys. The ESC Textbook of Cardiovascular Medicine (The European Society of Cardiology Series) Volume 1 & 2, 3rd Edition.
35. Banerjee I, Fuseler JW, Price RL, Borg TK, Baudino TA. Determination of cell types and numbers during cardiac development in the neonatal and adult rat and mouse. Am J Physiol Heart Circ Physiol. 2007 Sep;293(3):H1883-91. doi: 10.1152/ajpheart.00514.2007. Epub 2007 Jun 29. PMID: 17604329.
36. Caforio A.L., et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2013;34(33):2636–2648. doi: 10.1093/eurheartj/eht210. 2648a-2648d PMID: 23824828.
37. Cooper LT Jr. Myocarditis. N Engl J Med. 2009 Apr 9;360(15):1526-38. doi: 10.1056/NEJMra0800028. PMID: 19357408; PMCID: PMC5814110.
38. De Paris V, Biondi F, Stolfo D, et al. Pathophysiology. 2019 May 18. In: Sinagra G, Merlo M, Pinamonti B, editors. Dilated Cardiomyopathy: From Genetics to Clinical Management [Internet]. Cham (CH): Springer; 2019. Chapter 3.
39. Lampejo T, Durkin SM, Bhatt N, Guttmann O. Acute myocarditis: aetiology, diagnosis and management. Clin Med (Lond). 2021;21(5):e505-e510. doi:10.7861/clinmed.2021-0121.
40. Libby P, Swirski FK, Nahrendorf M. The Myocardium: More Than Myocytes. J Am Coll Cardiol. 2019 Dec 24;74(25):3136-3138. doi: 10.1016/j.jacc.2019.10.031. PMID: 31856970.
41. Lota AS, Halliday B, Tayal Uet al. Epidemiological trends and outcomes of acute myocarditis in the National Health Service of England. Circulation 2019;140:A11463.
42. Mahajan VS & Jarolim P. How to Interpret Elevated Cardiac Troponin Levels. Originally published 22 Nov 2011. https://doi.org/10.1161/CIRCULATIONAHA.111.023697. Circulation. 2011;124:2350–2354.
43. National Organization for Rare Disorders (NORD) https://rarediseases.org/rare-diseases/myocarditis/
44. Tran DB, Weber C, Lopez RA. Anatomy, Thorax, Heart Muscles. [Updated 2020 Sep 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/bookb/NBK545195/
45. Weinhaus A.J., Roberts K.P. (2009) Anatomy of the Human Heart. In: Iaizzo P. (eds) Handbook of Cardiac Anatomy, Physiology, and Devices. Humana Press. https://doi.org/10.1007/978-1-60327-372-5_5.
46. Myocarditis Foundation. Myocarditis Education Updates and How to Potentially Diagnose the Disease. Aug 4, 2020.
47. Myocarditis Foundation. Myocarditis in children: incidence, clinical characteristics and outcomes. Jul 29, 2020.
48. Mythili S, Malathi N. Diagnostic markers of acute myocardial infarction. Biomed Rep. 2015;3(6):743-748. doi:10.3892/br.2015.500.
49. Kociol R.D., Cooper L.T., Fang J.C., Moslehi J.J., Pang P.S., Sabe M.A., Shah R.V., Sims D.B., Thiene G., Vardeny O. Recognition and initial management of fulminant myocarditis: a scientific statement from the American heart association. Circulation. 2020; 141(6):e69–e92. doi: 10.1161/cir.0000000000000745. PMID: 31902242.
50. Krejci J., Mlejnek D., Sochorova D., Nemec P. Inflammatory cardiomyopathy: a current view on the pathophysiology, diagnosis, and treatment. Biomed Res Int, 2016. 2016:4087632. doi: 10.1155/2016/4087632. PMID: 27382566; PMC4921131.
51. Peretto G, et al. Arrhythmias in myocarditis: State of the art. Heart Rhythm. 2019 May;16(5):793-801. doi: 10.1016/j.hrthm.2018.11.024. Epub 2018 Nov 24. PMID: 30476544.
52. Ucar FM, Ozturk C, Yılmaztepe MA. Evaluation of Tp-e interval, Tp-e/QT ratio and Tp-e/QTc ratio in patients with acute myocarditis. BMC Cardiovasc Disord. 2019 Oct 22;19(1):232. doi: 10.1186/s12872-019-1207-z. PMID: 31640548; PMCID: PMC6805629.
53. Vaidyanathan R, O'Connell RP, Deo M, et al. The ionic bases of the action potential in isolated mouse cardiac Purkinje cell. Heart Rhythm. 2013;10(1):80-87. doi:10.1016/j.hrthm.2012.10.002.
54. https://www.cdc.gov/dhdsp/myocarditis.htm
55. https://www.mayoclinic.org/diseases-conditions/myocarditis/symptoms-causes/syc 20352539
56. Temporary_Authorisation_Patient_Information_BNT162_7_0_UK.pdf
57. Fact Sheet for Vaccination Providers-Full EUA PI_Final_2.25.2021.pdf
58. FDA News Release. FDA Approves First COVID-19 Vaccine. Approval Signifies Key Achievement for Public Health, August 23, 2021.
59. Corbett, K.S., Edwards, D.K., Leist, S.R. et al. SARS-CoV-2 mRNA vaccine design enabled by prototype pathogen preparedness. Nature 586, 567–571 (2020). https://doi.org/10.1038/s41586-020-2622-0.
60. Khan T, Agnihotri K, Tripathi A, Mukherjee S, Agnihotri N, Gupta G. Johns Hopkins University Coronavirus Resource Center. COVID-19 dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. 2020, CDC, WHO, COVID-19: A Worldwide, Zoonotic, Pandemic Outbreak. Altern Ther Health Med. 2020 Aug;26(S2):56-64. PMID: 32412918.
61. Ioannidis, J.P. (2021), Reconciling estimates of global spread and infection fatality rates of COVID‐19: an overview of systematic evaluations. Eur J Clin Invest. Accepted Author Manuscript e13554. https://doi.org/10.1111/eci.13554.
62. Malone, RW, Felgner, PL, Verma IM. Cationic liposome-mediated RNA transfection. Proceedings of the National Academy of Sciences (PNAS) 86 (16), 6077-6081.
63. Polack FP, et al. C4591001 Clinical Trial Group. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N Engl J Med. 2020 Dec 31;383(27):2603-2615. doi: 10.1056/NEJMoa2034577. Epub 2020 Dec 10. PMID: 33301246; PMCID: PMC7745181.
64. Rose, J. 2021. A report on the US Vaccine Adverse Events Reporting System (VAERS) of the COVID-19 messenger ribonucleic acid (mRNA) biologicals. Sci Publ Health Pol & Law .Volume 2:59-80.
65. Rose J. 2021. Critical Appraisal of VAERS Pharmacovigilance: Is the U.S. Vaccine Adverse Events Reporting System (VAERS) a Functioning Pharmacovigilance System? Sci Publ Health Pol & Law. Volume 3:100–129.
66. Tinari S. The EMA covid-19 data leak, and what it tells us about mRNA instability BMJ 2021; 372 :n627 doi:10.1136/bmj.n627.
67. Walsh EE, et al. Safety and Immunogenicity of Two RNA-Based Covid-19 Vaccine Candidates. N Engl J Med. 2020 Dec 17;383(25):2439-2450. doi: 10.1056/NEJMoa2027906. Epub 2020 Oct 14. PMID: 33053279; PMCID: PMC7583697.
68. Wolff JA, Malone RW, et al. Direct gene transfer into mouse muscle in vivo. Science. 1990;247(4949 Pt 1):1465-8.
69. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/specific-groups/allergies.html
70. https://www.cdc.gov/vaccines/covid-19/info-by-product/pfizer/reactogenicity.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fvaccines%2Fcovid-19%2Finfo-by-manufacturer%2Fpfizer%2Freactogenicity.html
71. https://ourworldindata.org
72. https://www.docdroid.net/xq0Z8B0/pfizer-report-japanese-government-pdf#page=17
73. https://phmpt.org/
74. Castiello T, Georgiopoulos G, Finocchiaro G, et al. COVID-19 and myocarditis: a systematic review and overview of current challenges. Heart Fail Rev. 2022;27(1):251-261. doi:10.1007/s10741-021-10087-9.
75. Fatmi SS, Basso R, Liaqat A, Tariq F, Swamiappan R. COVID-19 Myocarditis: Rationale for Early Diagnosis and Intervention. Cureus. 2021 Jul 19;13(7):e16494. doi: 10.7759/cureus.16494. PMID: 34430109; PMCID: PMC8373509.
76. Gregorio Tersalvi, MD, Marco Vicenzi, MD, Davide Calabretta, MD, Luigi Biasco, MD, PhD, Giovanni Pedrazzini, MD, Dario Winterton, MD. Elevated Troponin in Patients with Coronavirus Disease 2019: Possible Mechanisms. Review article| Volume 26, ISSUE 6, P470-475, June 01, 2020. Published: April 18, 2020. DOI:https://doi.org/10.1016/j.cardfail.2020.04.009.
77. Imazio M, Klingel K, Kindermann I, Brucato A, De Rosa FG, Adler Y, De Ferrari GM. COVID-19 pandemic and troponin: indirect myocardial injury, myocardial inflammation or myocarditis? Heart. 2020 Aug;106(15):1127-1131. doi: 10.1136/heartjnl-2020-317186. Epub 2020 Jun 4. PMID: 32499236.
78. Kariyanna P.T., Sutarjono B., Grewal E., Singh K.P., Aurora L., Smith L., Chandrakumar H.P., Jayarangaiah A., Goldman S.A., Salifu M.O., McFarlane I.M. A systematic review of COVID-19 and myocarditis. Am J Med Case Rep. 2020;8(9):299–305. PMID: 32747875; PMC7397751.
79. Liang Chen, Xiangjie Li, Mingquan Chen, Yi Feng, Chenglong Xiong, The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2, Cardiovascular Research, Volume 116, Issue 6, 1 May 2020, Pages 1097–1100, https://doi.org/10.1093/cvr/cvaa078.
80. Martinez MW, et al. Prevalence of Inflammatory Heart Disease Among Professional Athletes with Prior COVID-19 Infection Who Received Systematic Return-to-Play Cardiac Screening. JAMA Cardiol. 2021 Jul 1;6(7):745-752. doi: 10.1001/jamacardio.2021.0565. PMID: 33662103; PMCID: PMC7934073.
81. Mele D, Flamigni F, Rapezzi C, Ferrari R. Myocarditis in COVID-19 patients: current problems. Intern Emerg Med. 2021 Jan 23:1–7. doi: 10.1007/s11739-021-02635-w. Epub ahead of print. PMID: 33484452; PMCID: PMC7823176.
82. Nascimento JHP, Gomes BFO, Oliveira GMM. Cardiac Troponin as a Predictor of Myocardial Injury and Mortality from COVID-19. Arq Bras Cardiol. 2020 Oct;115(4):667-668. English, Portuguese. doi: 10.36660/abc.20200862. PMID: 33111867.
83. Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, Shchendrygina A, Escher F, Vasa-Nicotera M, Zeiher AM, Vehreschild M, Nagel E. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020 Nov 1;5(11):1265-1273. doi: 10.1001/jamacardio.2020.3557. Erratum in: JAMA Cardiol. 2020 Nov 1;5(11):1308. PMID: 32730619; PMCID: PMC7385689.
84. Sawalha K., Abozenah M., Kadado A.J., Battisha A., Al-Akchar M., Salerno C., Hernandez-Montfort J., Islam A.M. Systematic review of COVID-19 related myocarditis: insights on management and outcome. Cardiovasc Revascularization Med. 2021;23:107–113. doi: 10.1016/j.carrev.2020.08.028. PMID: 32847728; PMC7434380.
85. Singer ME, Taub IB, Kaelber DC. Risk of Myocarditis from COVID-19 Infection in People Under Age 20: A Population-Based Analysis. medRxiv [Preprint]. 2021 Jul 27:2021.07.23.21260998. doi: 10.1101/2021.07.23.21260998. PMID: 34341797; PMCID: PMC8328065.
86. Siripanthong B, Nazarian S, Muser D, et al. Recognizing COVID-19-related myocarditis: The possible pathophysiology and proposed guideline for diagnosis and management. Heart Rhythm. 2020;17(9):1463-1471. doi:10.1016/j.hrthm.2020.05.001.
87. Vogel G., Couzin-Frankel, J. Israel reports link between rare cases of heart inflammation and COVID-19 vaccination in young men. Jun. 1, 2021.
88. How Can COVID-19 Affect the Heart? Aug 18, 2020. Myocarditis Foundation
89. VAERSDataUseGuide_November2020
90. Vaccine Adverse Event Reporting System (VAERS), Standard Operating Procedures for COVID-19 (as of 29 January 2021) VAERS Team: Immunization Safety Office, Division of Healthcare Quality Promotion National Center for Emerging and Zoonotic Infectious Diseases and Centers for Disease Control and Prevention.
91. NIA Adverse Event and Serious Adverse Event Guidelines
92. https://www.meddra.org/
93. Lazarus, Ross et al. Grant Final Report. Grant ID: R18 HS 017045. Electronic Support for Public Health–Vaccine Adverse Event Reporting System (ESP:VAERS). Submitted to The Agency for Healthcare Research and Quality (AHRQ).
94. Guetzkow. J. Adverse Events Reported Following COVID-19 Vaccinations. https://tinyurl.com/CovidvFluReport.
95. Noa Dagan, M.D., et al. BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Mass Vaccination Setting. New England Journal of Medicine. February 24, 2021, DOI: 10.1056/NEJMoa2101765.
96. Rose, J. & McCullough P. 2021. A Report on Myocarditis Adverse Events in the U.S. Vaccine Adverse Events Reporting System (VAERS) in Association with COVID-19 Injectable Biological Products. In Review. Submitted to Reviews in Cardiovascular Medicine.
97. Shimabukuro, T. COVID-19 Vaccine safety updates. Advisory Committee on Immunization Practices (ACIP). CDC COVID-19 Vaccine Task Force. June 23, 2021.
98. Tracy Beth Høeg, Allison Krug, Josh Stevenson, John Mandrola. SARS-CoV-2 mRNA Vaccination-Associated Myocarditis in Children Ages 12-17: A Stratified National Database Analysis. medRxiv 2021.08.30.21262866; doi: https://doi.org/10.1101/2021.08.30.21262866.
99. McCullough PA, et al. Pathophysiological Basis and Rationale for Early Outpatient Treatment of SARS-CoV-2 (COVID-19) Infection. Am J Med. 2021 Jan;134(1):16-22. doi: 10.1016/j.amjmed.2020.07.003. Epub 2020 Aug 7. PMID: 32771461; PMCID: PMC7410805.
100. McCullough PA, et al. Multifaceted highly targeted sequential multidrug treatment of early ambulatory high-risk SARS-CoV-2 infection (COVID-19). Rev Cardiovasc Med. 2020 Dec 30;21(4):517-530. doi: 10.31083/j.rcm.2020.04.264. PMID: 33387997.
101. McCullough PA, Vijay K. SARS-CoV-2 infection and the COVID-19 pandemic: a call to action for therapy and interventions to resolve the crisis of hospitalization, death, and handle the aftermath. Rev Cardiovasc Med. 2021 Mar 30;22(1):9-10. doi: 10.31083/j.rcm.2021.01.301. PMID: 33792243.
Supplementary Materials
Supplementary Table 1
Supplementary Table 2
Supplementary Table 3
List of VAERS IDs with clear pathognomonic markers for COVID-19 vaccine-induced myocarditis
VAERS ID: 1486983; 13 years old; 1 day after 2nd shot. “Troponin I 5.23 (7/19@1936), 5.08 (7/19@2014), 3.63 (7/20@0215). C-Reactive Protein 10.2 (7/20@0806), BNP 24 (7/19@1936). [Chest pain.] COVID Negative.”
VAERS_ID: 1693372. 31 years old. myocarditis developed 2 days after the 2nd shot. troponin almost 22K. No history. No illnesses. No meds.
VAERS_ID: 1533287. 12 years old. Chest pain. hs troponin peak at >25,000 ng/L Echo normal
VAERS_ID: 1539671. 15 years old. CHEST PAIN, ELEVATED TROPONIN >22,000 WITH EKG CHANGES, SUSPECTED MYOCARDITIS
VAERS_ID: 1974116. 17 years old. Troponin 9,986.9, then 15,943.8
VAERS_ID: 2019971. 33 years old. high sensitivity troponin 28k (elevated) EKG with diffuse ST elevation and PR depression
VAERS_ID: 1327111. 19 years old. CRP increased. Troponin 10.804 CRP 32 Echocardiogram ordered for LV function.
VAERS_ID: 1962935. 26 years old. high-sensitivity troponin 1,387 (myocarditis) EKG with diffuse ST elevations and PR depressions (pericarditis).
VAERS_ID: 1334092. 23 years old. Chest pain. Troponin peak of 6 CRP >100 MRI showed subepicardial gadolinium enhancement in the basal inferolateral wall.
VAERS_ID: 1357884. 16 years old. CBC - nl, d-dimer elevated at 0.60, troponin 6,389, CRP 9.50, ESR 22, BNP 479 EKG Sinus rhythm , ST elevation II, III, aVF, V4-V6 and ST depression with T wave inversions
VAERS_ID: 1394876. 14 years old. normal Echocardiogram 6/13/2021--elevated highly sensitive troponin at over 1000 ng/L
VAERS_ID: 1487493. 22 years old. B-Natriuretic Peptide: 12 CK: 163 CK MB: 3.3 CRP hs Cardiac: 0.92 Troponin I:1554 (!) Myoglobin: 46. COVID-19 vaccine induced myopericarditis.
VAERS_ID: 1493763. 15 years old. Troponin 20,987 at 1450 and CRP 79.4. 7/17 Troponin 28,338 at 2336. 7/18 Troponin 23376, CRP 53. 7/19 Troponin 19,463, CRP 29. 7/20 Troponin 4,658, CRP 16.6.
Supplementary Table 4
Supplementary Table 5
Supplementary Figure 1
Supplementary Figure 2
Supplementary Figure 3
[1] Myocarditis can manifest as sudden death, chest pain or heart failure. The symptoms of heart failure from myocarditis include effort intolerance, dyspnea, fatigue, and ankle swelling.
[2] mRNA injectable products (biologicals) are not true vaccines. True vaccines are a preparation of a weakened or killed pathogen, such as a bacterium or virus, or of a portion of the pathogen's structure that upon administration to an individual stimulates antibody production or cellular immunity against the pathogen but is incapable of causing severe infection. Vaccines undergo an extremely rigorous testing time-dependent protocol to ensure safety and efficacy typically enduring between 10 and 15 years. The mRNA biologicals do not satisfy either these requirements and are thus more akin to experimental gene therapy.
[3] The COVID-19 vaccines administered in the U.S. have not been approved or licensed by the U.S. Food and Drug Administration (FDA), having been authorized instead for emergency use by FDA under an Emergency Use Authorization (EUA), originally designed to prevent Coronavirus Disease 2019 (COVID-19) for use in individuals 16 years of age and older.
[4] It must be noted that the reported AEs as part of the VAERS represent a fraction of the actual number of incidents. Studies have shown that the percentage of incidents reported can be quite low (1-10%) but, for the purposes of this report, in order to do the necessary calculations, VAERS numbers were used, and the results should be considered to reveal trends.
[5] These classifications are based on the Code of Federal Regulations. The VAERS handbook states that approximately 15% of reported AEs are classified as severe.
[6] Dr. Rochelle Walensky, director of the Centers for Disease Control and Prevention
[7] John R. Su, MD, PhD, MPH, Vaccine Safety Team, CDC COVID-19 Vaccine Task Force. ACIP presentation October 21, 2021.
[8] The cardinal signs of myocarditis determined by an echocardiogram include an elevated wall thickness, dilation, pericardial effusion, and ventricular systolic dysfunction. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8270733/
[9] Daniels CJ, Rajpal S, Greenshields JT, et al. Prevalence of Clinical and Subclinical Myocarditis in Competitive Athletes With Recent SARS-CoV-2 Infection: Results From the Big Ten COVID-19 Cardiac Registry. JAMA Cardiol. 2021;6(9):1078-1087. doi:10.1001/jamacardio.2021.2065.
[10] In cases where the echocardiogram is unrevealing, cardiac Magnetic Resonance Imaging (MRI) can detect changes in tissue characterization consistent with myocardial inflammation.
[11] https://vaers.hhs.gov/data/datasets
[12] Medical Dictionary for Regulatory Activities https://www.meddra.org/
[13] Since VAERS reports of AEs related to cardiac inflammation can span a variety of MedDRA code classifications such as ‘Myopericarditis’, ‘Myocarditis’ and ‘Autoimmune myocarditis’ as prominent examples, for the purposes of this study so as not to exclude potential myocarditis cases, a function was created to select specific key words to capture these cases.
[14] MYOCARDITIS STRING - according to ACIP October 21,2021 report (https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-10-20-21/07-COVID-Su-508.pdf)
[15] Hannah Ritchie, Edouard Mathieu, Lucas Rodés-Guirao, Cameron Appel, Charlie Giattino, Esteban Ortiz-Ospina, Joe Hasell, Bobbie Macdonald, Diana Beltekian and Max Roser (2020) - "Coronavirus Pandemic (COVID-19)". Published online at OurWorldInData.org.
[16] https://usafacts.org/visualizations/covid-vaccine-tracker-states/
[17]A COVID Case is defined by the keywords: "Pneumonia viral", "COVID-19", "Suspected COVID-19", "SARS-CoV-2 test positive", "COVID-19 pneumonia", "Asymptomatic COVID-19", "Vaccine breakthrough infection"
[18] It is important to note that this might mean that more youths were tested with higher frequency for these markers in association with myocarditis. It is highly unlikely that this is the case, but it warrants mentioning. It is not possible to know with certainty.
[19] At least 254,599,776 people or 77% of the population have received at least one dose. Overall, 216,690,804 people or 65% of the population are considered fully vaccinated. Additionally, 96,035,748 people or 29% of the population have received a booster dose. https://usafacts.org/visualizations/covid-vaccine-tracker-states/
[20] Nassar M, Nso N, Gonzalez C, et al. COVID-19 vaccine-induced myocarditis: Case report with literature review [published correction appears in Diabetes Metab Syndr. 2021 Sep-Oct;15(5):102277]. Diabetes Metab Syndr. 2021;15(5):102205. doi:10.1016/j.dsx.2021.102205
[21] https://wonder.cdc.gov/vaers.html
[22] https://www.cdc.gov/flu/season/faq-flu-season-2020-2021.htm
[23] N.B. These counts do not represent the individuals who experienced an AE but the total number of events reported.
[24] https://www.cdc.gov/coronavirus/2019-ncov/vaccines/safety/myocarditis.html



Today my husband attended a small conference for investors hosted by a wealth mgmt group, here in the Uk. Over lunch, one of the wealth mgmt advisors spoke to my husband and discussed the adverse event and deaths post jab, the WEF, klaus Schwab, food shortages, cost of living increases, skyrocketing petrol prices etc etc. It is no longer the belief of professionals such as you and Dr. Peter McCullough who believe these experimental biologicals are a danger because they cause serious adverse events and deaths. Mainstream non healthcare professionals are now having the same discussions and concerns. This is what was needed. These “others” are expressing their concerns about the narrative and asking questions.
this is so well done and so incredibly through, even those of us with basic knowledge of statistics can see the conclusiveness of this! One can't see how ANY scientific journal or serious scientist could possibly refute this. if/when they do, it will only prove how dishonest and corrupt THEY are. real science isn't dead, just buried under loads of money and greedy bull****!